
Top 10 Medical Billing Companies in Yonkers, NY
“Transcure leads the list of top medical billing companies in Yonkers, New York, with its AI-driven automation that improves accuracy and speeds up payments. Alongside
|
|
Thank you for Signing Up |


Accurate coding and billing to reduce denials and boost revenue cycle efficiency.

Custom billing support designed to help small practices grow and get paid faster.

We identify billing gaps and errors to improve compliance and maximize revenue.

A medical billing company that understands the unique needs of your specialty.

Trusted by
500+ Physicians

Catering to
40+ Specialties

1100+ Certified
Medical Billers & Coders

End-to-End
RPA Billing Solutions

Up to 98% First Pass
Clean Claim Rate
Our medical billing company simplifies every step of the billing cycle to help practices get paid faster, with fewer denials.
We evaluate your workflows, goals, and specialty needs to personalize billing.
We gather patient details and verify insurance coverage upfront
Certified coders assign precise CPT, ICD, and HCPCS codes for clean claims.
Claims are submitted electronically to minimize delays and rejections.
We post payments from payers and patients, ensuring accurate tracking.
You receive timely payouts and detailed performance reports for full visibility.
ELIXA transforms eligibility verification with intelligent medical billing automation. It connects to EHRs and payer systems via EDI, APIs, and AI-driven calls to interpret coverage data in real time. It even shows the number of eligibility checks that required prior authorization.
On its dashboard, you can see Live AI Activity to analyze the eligibility verification status happening through billing automation. It even tracks claim details and verification trends.

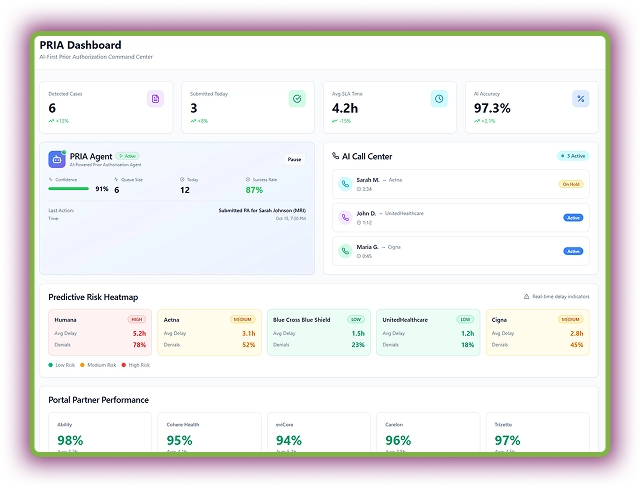
PRIA automates case detection and payer follow-ups with over 97% accuracy. Its Predictive Risk Heatmaps identify high-risk denials before they happen. Moreover, the AI Call Center automates payer calls to drastically reduce manual phone time spent on getting status updates or submitting verbal PAs.
Within the dashboard, you can track integration performance with different payer portals. This agent gives AI confidence in its decision to show it has selected the correct payer.
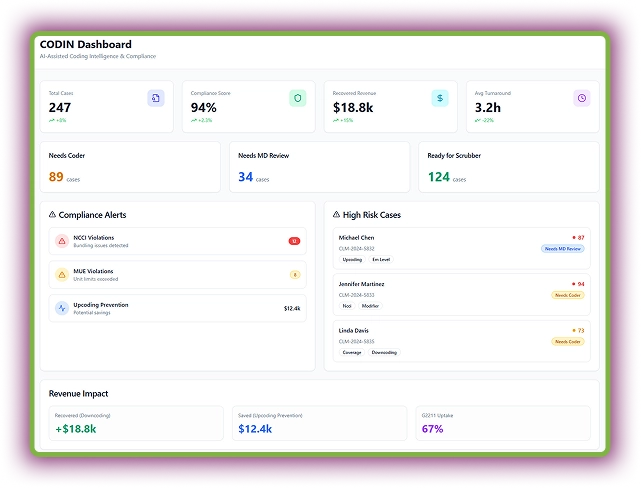
CODIN automates medical coding with AI that reads clinical notes, extracts diagnoses, and procedures. After extracting data points with its OCR technology, matches them to the correct CPT and ICD codes. It audits every claim, detecting NCCI or MUE violations and flagging missing documentation.
Moreover, this medical billing automation agent analyzes prepared claims to suggest the right codes for higher reimbursements.
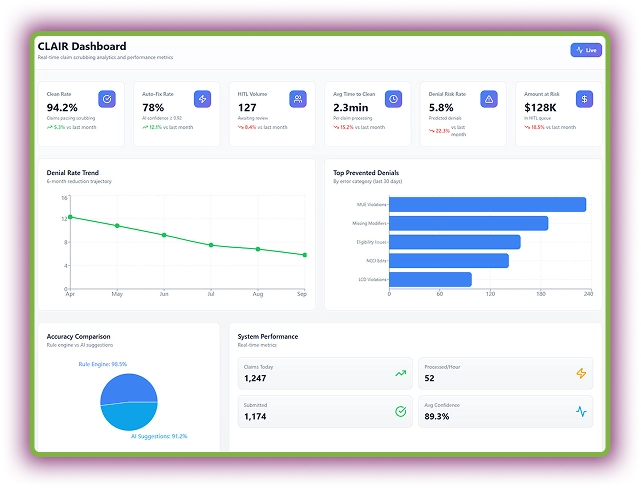
CLAIR is your intelligent claim scrubbing AI agent designed to eliminate denials before they happen. It analyzes claim line items (codes, modifiers, coverage, provider info) using AI and payer rules. The dashboard even displays live clean rates, denial trends, and system accuracy.
Surprisingly, this AI agent auto-fixes minor issues like modifier errors or code mismatches using trained models. Moreover, it compares each claim against historical denial patterns.
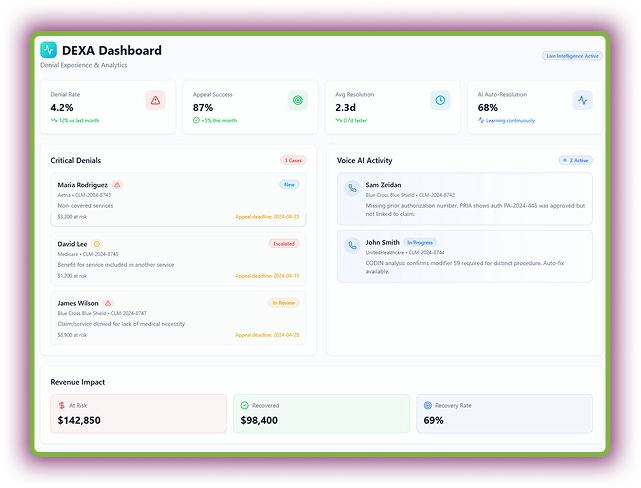
DEXA revolutionizes denial management by turning payer rejections into revenue opportunities. This AI agent detects, analyzes, and resolves denials in real time. DEXA documents each call outcome in real time and updates claim statuses automatically in the EHR or billing software.
More importantly, this AI RCM tool auto-categorizes critical denials, generates appeal letters, and even calls payers to verify claim details.
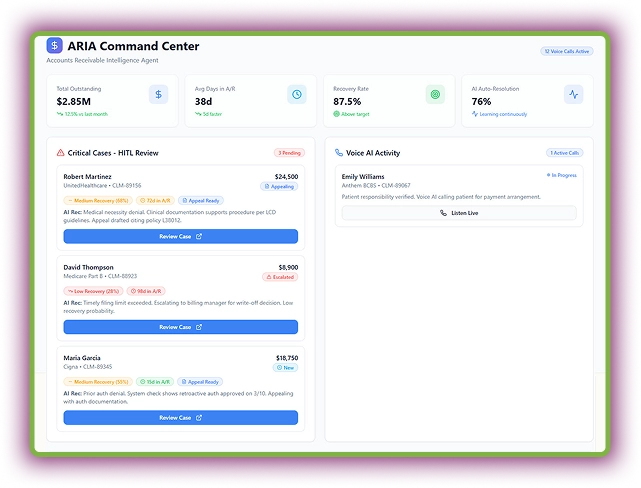
ARIS intelligently tracks outstanding claims and auto-drafts appeals using payer-specific rules. Its predictive engine scores recovery probability, prioritizing the highest-value accounts for faster action. Moreover, Voice AI handles patient payment calls to improve payment collection.
With real-time payer performance insights, ARIS empowers teams to make smarter recovery decisions. Most of the appeals and billing-related escalations are fully automated.
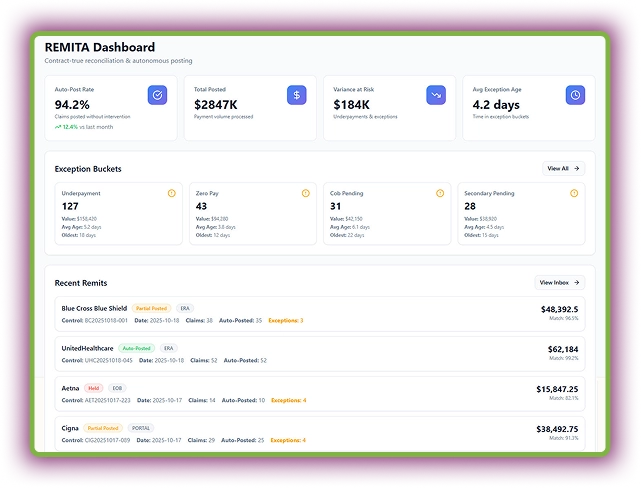
REMITA is an AI automation tool for payment reconciliation and exception management in the healthcare RCM. This AI billing agent auto-reconciles remittance data (ERAs and EOBs) with expected payments and posts payments automatically to patient and insurance accounts.
Plus, this agent detects and flags exceptions, such as underpayments, denials, or missing info. Overall, it reduces manual intervention by continuously learning payer patterns.
Our medical billing company cater to a wide range of specialties, spanning from primary care to surgical centers, serving small and mid-sized practices.
Our medical billing specialists know the workarounds of all the EHRs. We help you submit clean claims no matter which EHR you use.
Our Certifications
We strictly adhere to compliance and state regulations and our certifications exhibit that well.





Transcure is redefining what it means to be a medical billing company in the U.S. With a strong presence in all the major states and growing, our mission is to deliver specialty-driven medical billing services that adapt to each region’s unique healthcare requirements.
Get the latest healthcare industry insights to learn more about making your practice more profitable.
Discover health IT news and learn more about the ongoing trends around you with our article hub!
Discover how Transcure has helped medical practices overcome their billing challenges.
Make informed decisions about your practice success with real-time feedback. Explore Clients’ thoughts!
Explore the latest healthcare industry insights to enhance practice performance and profitability.

“Transcure leads the list of top medical billing companies in Yonkers, New York, with its AI-driven automation that improves accuracy and speeds up payments. Alongside

“The best medical billing companies in Islip, NY include Transcure, recognized for its AI-powered billing platform and dedicated AI agents. This innovation helps local practices

Compare the top medical billing companies in Buffalo like Transcure, Buffalo Billing, iRCM, and choose the best suits your practice’s needs.
|
|
Thank you for Signing Up |

A medical billing company is an intermediary between healthcare providers, patients, and insurance payers. It helps your practice get paid by generating, submitting, and tracking medical claims for maximum and timely revenue collection.
Our team of certified billers and coders has expertise in more than 40 specialties that ensures personalized medical billing services for your practice.
We offer flexible pricing. You can choose the percentage of the collection pricing model with no hidden costs.
Yes, we can work with the billing software you currently use. Our team will conduct a brief demo and familiarize itself with your system for better service delivery.