Electronic Health Records (EHR) have become an integral part of modern medical practices today. Any practice that requires an organized and efficient billing workflow must implement a reliable EHR system. However, over 500 EHR vendors are available, which makes it challenging to decide which system is best for your practice.
Among all EHRs, Athenahealth is a leading choice due to its ease-of-use and cloud-based workflow. With data from over 140,000 clinicians and thousands of healthcare associations across the country, Athenahealth is one of the largest repositories of patient data in the U.S.
Before using Athenahealth, practices need to completely understand how it works and how it fits into their financial operations. This guide explores what Athenahealth EHR is, how it links to medical billing, and why partnering with an expert Athena billing company helps practices use it effectively.

Table of Contents
ToggleIntroduction to Athenahealth EHR
It’s important to first know what Athenahealth is and how it functions to fully understand how it supports healthcare practice. This Athena EMR cheat sheet provides a clear overview of Athenahealth EHR and its key features.
What is Athenahealth EHR?
Athenahealth is a cloud-based electronic health record (EHR) system that is designed to help healthcare providers improve patient care. Since it’s cloud based, it can be accessed from any location with an internet connection. This makes it ideal for healthcare providers who need to access patient records from multiple locations.
Athenahealth EHR is preferred by healthcare facilities due to its ability to bring clinical documentation, scheduling, practice management, and billing together into one connected system. This EHR system is also interoperable, meaning it can integrate with other practice management software, such as laboratory systems, imaging systems, and medical billing systems.
Purpose and Role in Healthcare Administration
Automation of Patient Records: Athenahealth EHR replaces paper charts, digitizing patient information for easier access and management.
Enhanced Care Coordination: Allows multiple clinicians to collaborate in real time within a single patient chart for seamless continuity of care.
Improved Safety and Quality: According to CMS, Athenahealth EHR reduces duplicate tests, delays, and errors by providing up-to-date health data.
Support for Workflows: Athenahealth helps manage scheduling, e-prescribing, and clinical documentation efficiently.
Mobile and Remote Access: Supports documentation and virtual visits through mobile devices, enabling flexibility for providers and accessibility for patients.
Regulatory Compliance: The system helps practices in meeting reporting requirements and quality standards.
Centralized Patient Information: Demographics, medical histories, allergies, medications, and visit notes are all stored in one place.
How Athenahealth EHR Fits into the Healthcare Revenue Cycle
Patient Registration
Athenahealth simplifies patient onboarding and appointment booking to ensure the collection of demographic and insurance information is accurate.
Insurance Verification
The system automates the insurance verification and eligibility process, allowing providers to verify coverage information quickly.
Clinical Documentation
Athenahealth’s EHR enables precise and effective clinical documentation, which is crucial for correct coding and billing.
Charge Capture
This platform streamlines charge capture and claim submission procedures to guarantee prompt and precise billing.
Denial Management
Athenahealth allows for effective tracking and management of claim denials, helping practices to address the issues and resolve them on time.
Payment Posting
With Athenahealth, payments are posted and reconciled automatically that helps in reducing errors and ensuring precise financial tracking.
Reporting Tools
Practices can track financial performance and pinpoint areas needing attention using Athenahealth analytics and reporting tools.
Patient Billing
Automated patient invoicing and collections tools improve the billing experience, making it easier for patients to understand their financial responsibilities and make payments.

How Athenahealth EHR Connects with Medical Billing
Athenahealth’s athenaOne platform integrates Electronic Health Records (EHR) with medical billing to ensure patient data flows smoothly from documentation to billing without errors. Here are some of the ways through which Athenahealth EHR connects with medical billing.
Patient Data and Documentation Flow into Billing
When patient visits are documented in Athenahealth’s EHR, the information flows into the billing process. Visit notes, procedure orders, and diagnoses entered by clinicians are automatically added to the charge capture section.
Athenahealth also automatically suggests Athena billing codes such as CPT and ICD codes based on the clinician’s notes or orders. This level of integration means that accurate patient histories, labs, and physician observations all feed directly into code assignment.
Reducing Errors through Accurate Records
In Athenahealth EHR, clinicians input data electronically or through templates. This reduces the risk of errors due to unclear handwriting or missing information. Additionally, the system can detect inconsistencies immediately, like, if a code doesn’t match a documented procedure, the system will alert the user.
Moreover, Athenahealth has built-in coding tools that help billers follow the latest ICD-10 rules. This EHR system also has alerts called diagnosis-gap alerts that point out any conditions or information that might be missing.
Coordination between Clinical and Financial Workflows
Athenahealth’s all-in-one platform increases coordination between clinical teams and the practice’s revenue-cycle staff. As physicians, nurses, and coders all access the same networked records, communication gaps are reduced.
Billing staff can easily access reports on unpaid claims or patient balances and refer back to patient charts in Athenahealth for clarification. Similarly, providers can see billing updates, like claim denials or payments within the patient record.
How Transcure Supports Practices Using Athenahealth EHR for Billing
Transcure is a medical billing and AthenaHealth RCM services provider that specializes in Athenahealth EHR practices. They offer end-to-end Billing services for Athena EHR and some of the key aspects of their services are discussed below:
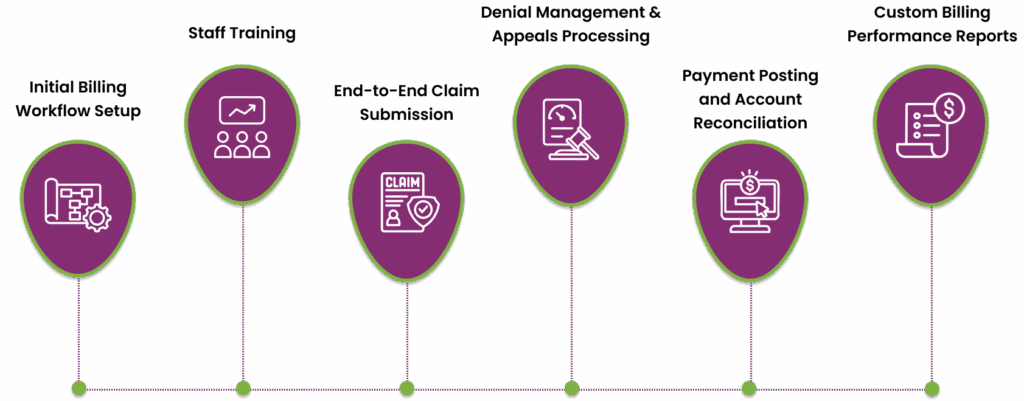
Initial Billing Workflow Setup within Athenahealth EHR
Transcure consultants help practices set up Athenahealth for smooth and accurate billing. They configure important features like payer portals, fee schedules, provider profiles, and visit templates to fit the practice’s needs.
While Athenahealth offers general training, Transcure fine-tunes these settings so that all billable services are captured correctly. For example, they adjust charge pools or visit types to make sure every patient encounter generates the right billing entry automatically. This setup ensures that billing is consistent for every visit.
Staff Training on Billing Functions in Athenahealth
Transcure provides targeted training for office and billing staff to fully use Athenahealth’s features. Their training covers how to enter and code encounters in Athenahealth, verify insurance eligibility, and use the EHR’s claim scrubbing tools.
Continuous education is prioritized so that coders and billers stay updated with both Athenahealth updates and payer requirements. The company conducts workshops or provides reference guides on Athenahealth’s charge entry screens and denial management system.
End-to-End Claim Submission and Tracking
Once clinical data is entered in Athenahealth, Transcure’s team handles the full claim cycle. They review each claim using Athenahealth’s claims dashboard and EDI tools to electronically submit to payers. The company also prioritizes proactive claim management by using Athenahealth’s rules engine and their own in-house scrubbing to prevent common errors.
After sending claims, Transcure monitors their status daily within Athenahealth’s system and generates follow-ups as needed. They also generate daily, weekly, and monthly reports on claim statuses.
Denial Management and Appeals Processing
In situations where denials or rejections occur, Transcure handles the appeals process within the Athenahealth workflow. They have an expert denial management approach in place that identifies denial trends and takes proactive actions to correct them.
The denial management experts then correct and resubmit claims through Athenahealth, or prepare appeals if needed. Also, Transcure has a rapid turnaround with denial resubmissions within 48 hours.
Payment Posting and Account Reconciliation
Transcure makes sure that all payments from insurance companies are correctly added to patient accounts in Athenahealth. When electronic payment reports arrive, the team reviews and records them in the system.
Any adjustments in the patient’s share or insurance write-offs, are also added so that account balances match the payment details. If there are differences, Transcure investigates and follows up on underpayments. This process is important because it completes the claim cycle and keeps accounts receivable accurate.
Custom Billing Performance Reports
Another major benefit of outsourcing Athenahealth billing services with Transcure is visibility. They provide Athenahealth clients with custom dashboards and reports that summarize billing performance. These reports track key performance metrics like days in A/R, denial rates, and net collections.
Reviewing these reports helps practices spot areas where errors may occur and make improvements. In addition, the dashboard includes graphical representations of accounts receivable and collectibles, which makes it easier for clients to understand the financial data.

Key Strengths of Transcure’s Medical Billing Services for Athenahealth EHR Users
Transcure enhances the efficiency of Athenahealth practices by combining expert billing knowledge with advanced technology. Here are the core strengths that set them apart:
- High First-Pass Claim Acceptance: Transcure helps Athenahealth EHR users achieve a 99% first-pass clean claim rate. This is due to their accurate charge entry and coding quality checks.
- Minimized Days in A/R: The company report accounts receivable are typically cleared within about 24 days. Rapid follow-up on unpaid claims means revenue comes in faster.
- Expertise Across Specialties: Transcure’s team includes over 1,100 Athena-trained billers and coders skilled in more than 30 specialties. The billers understand the specific coding and payer rules for all specialties.
- Scalable Billing Support: With cloud-based tools, Transcure can easily scale services as your practice grows. Practices, from independent to multi-speciality large health facilities can rely on their Athena medical billing services.
- HIPAA-Compliant, Secure Processes: All of Transcure’s operations follow HIPAA-compliant and ISO 27001 regulations. This ensures that patient information in Athenahealth’s EHR is handled with privacy during the billing process.
- Ongoing Workflow Optimization: Transcure doesn’t just process claims, they continuously improve workflows. By using Athenahealth’s reporting and Transcure’s analytics, they recommend process changes and training updates.

Summary: Athena EHR and Medical Billing in Modern Healthcare
Integrated EHR systems like Athenahealth strengthen care and financial operations simultaneously by digitizing patient records and linking them to billing platforms. Athenahealth’s cloud-based model and interoperability further ensure that data flows to where it’s needed that supports both clinical decisions and administrative tasks.
In order to get the best results from Athenehealth, specialized Athena EMR billing support is also vital. Expert billing companies like Transcure help practices make the most of Athenahealth’s features without getting stuck in the complicated details of revenue cycle management.
Practices using such integrated solutions often see big financial improvements. For example, Transcure reports that partnering with their Athena billing experts can increase revenues by around 20% while cutting costs by up to 25%. In summary, Athenahealth’s EHR and its integrated billing workflows when optimized by experienced partners can improve both operational efficiency and financial performance.
FAQs
What is the pricing structure of Athenahealth EHR?
Athenahealth EHR charges a percentage of what your practice earns, so they only get paid when you do. The pricing is transparent, with no hidden fees, low upfront costs, and no long-term contracts.
Which is the best Athena billing services provider in the U.S?
Transcure is considered one of the best Athena billing service providers in the U.S. due to its deep expertise in Athena EHR systems and nationwide reach across all 50 states.
Who can benefit from Athenahealth EHR?
Athenahealth EHR is ideal for small to medium-sized medical practices, specialty clinics, and large healthcare organizations.
Does Athenahealth handle insurance or payer communication?
Yes, Athenahealth manages insurance and payer communication by automating modifier applications and applying custom rules based on payer requirements. It also maintains a global rules library to ensure compliance with payer, state, and national regulations.









