Pulmonology billing is complex in the U.S., and managing it poorly can strain a practice’s finances. Between complex codes, denial management, and CMS updates, getting paid is harder than it should be. One glance at how many ICD and CPT codes you must juggle, and you realize why proper billing workflow isn’t optional.
In fact, over 62% of physicians worry about their practice’s financial stability, which highlights how important efficient revenue cycle management (RCM) is. Couple it with the fact that the average claim denial rate in pulmonary medicine stands at an alarming 18%. It is a figure that is significantly higher than the median rate of 5 to 10% for other medical specialties.
Breakdowns like this are exactly why you should read this guide to nail pulmonology medical billing and coding, and find a partner who can simplify everything. This guide explains the steps, challenges, and best practices, including how a specialized firm providing pulmonology billing services can help you get paid fully and on time.
Table of Contents
ToggleWhy RCM Matters for Pulmonology Practices
Effective revenue cycle management (RCM) is critical for pulmonologists because it ensures steady cash flow and regulatory compliance. Advanced billing systems and expert coding can reduce denials and accelerate collections, so providers aren’t left waiting months for reimbursement. Moreover, RCM safeguards compliance with U.S. laws and payer rules.
For instance, HIPAA imposes strict data and privacy standards, and violations can trigger huge fines. Likewise, Medicare’s own statutes (Social Security Act) forbid payment of any claim that “lacks the necessary information to process the claim.” In practice, this means every pulmonary function test (PFT), E/M note, and equipment order must be fully documented, or the claim is denied.
Plus, CMS’s Merit-based Incentive Payment System (MIPS) now includes a Pulmonology Value Pathway (2025) focused on COPD, asthma, sleep apnea, etc. This means accurate coding now affects incentive payments. In short, a streamlined pulmonology RCM is the backbone of financial health, as it preserves revenue and ensures compliance.

Process of Pulmonology Billing
Pulmonology billing follows a multi-step RCM workflow tailored to respiratory practices. Key steps include:
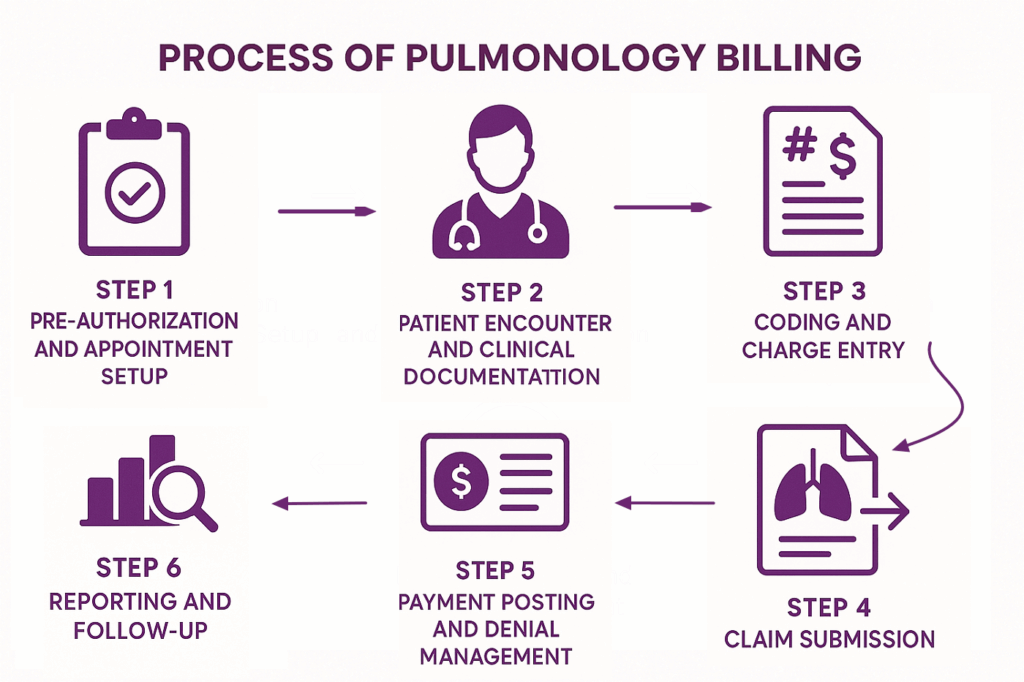
Step 1. Pre-Authorization and Appointment Setup
The billing cycle begins even before the patient walks in. Pulmonology practices must verify insurance eligibility and determine if prior authorization is required for procedures like bronchoscopy or PAP device setup. This prevents unexpected denials later. Please note that authorization details should always be logged in the EHR system for billing compliance.
Key actions in this step are:
- Check eligibility and benefits before scheduling
- Secure pre-authorization for high-cost procedures
- Record authorization numbers in the system
Step 2. Patient Encounter and Clinical Documentation
Accurate clinical documentation is the backbone of clean claims. During the visit, providers must capture medical necessity, procedure details, and interpretation of results. For rehab or sleep studies, documenting time spent and provider supervision is important. Most payer denials occur at this stage due to missing small elements, like calibration data in PFTs.
Key actions in this step are:
- Collect insurance and demographics at check-in
- Document the indication, procedure, and results clearly
- Ensure time and supervision notes are included
Step 3. Coding and Charge Entry
After services are provided, coders translate them into CPT and ICD-10 codes. This step demands special precision since many procedures overlap with E/M services. Modifiers such as 25 help separate significant visits from testing. Moreover, coders must cross-check entries against NCCI edits and payer LCDs for compliance to avoid claim rejections.
Key actions in this step are:
- Assign correct CPT and ICD-10 codes
- Use modifiers appropriately (e.g., 25 with spirometry)
- Validate codes against payer-specific policies
Example Table: Common Pulmonology Procedures
| Procedure | CPT Code | Example ICD-10 Codes (Medical Necessity) | Notes |
|---|---|---|---|
| Spirometry | 94010 | J44.9 (COPD), J45.909 (Asthma, unspecified) | Requires modifier 25 if billed with E/M |
| Bronchoscopy with biopsy | 31625 | J18.9 (Pneumonia, unspecified), R91.1 (Nodule) | Document site, specimen, complications |
| Pulmonary stress test | 94618 | J44.1 (COPD w/ exacerbation) | LCD requires detailed documentation |
| Pulmonary rehab, single session | G0237 | J44.9, J98.4 (Other pulmonary disorders) | Must record time and supervising MD |
| PAP device initial setup | E0601 | G47.33 (OSA) | Needs sleep study and DME compliance |
Step 4. Claim Submission
Once charges are finalized, claims are submitted electronically through clearinghouses or payer portals. Pulmonology claims often require additional documents, like sleep study reports for PAP devices or detailed rehab notes for G0237. Since each payer enforces unique rules, including visit caps or supply frequency limits, it is better to tailor submissions to prevent automatic denials.
Key actions in this step are:
- Submit claims electronically for faster processing
- Attach necessary supporting documentation
- Follow payer-specific coverage rules
Step 5. Payment Posting and Denial Management
In most cases, Pulmonology denials arise from missing modifiers, incomplete rehab documentation, or non-covered PAP supplies. Each denial should be reviewed, corrected, and appealed with proper medical necessity evidence. That’s because quick resolution keeps revenue steady and improves cash flow predictability.
Key actions in this step are:
- Post payments and reconcile with expected fees
- Identify common denial categories
- Appeal with proper documentation and LCD references

Step 6. Reporting and Follow-Up
The final step is monitoring the revenue cycle for patterns. Practices should track denial percentages, clean claim rates, and days in A/R. Regular reporting highlights where revenue is leaking, such as missed bronchoscopy add-ons or unbilled DME. Apart from that, quarterly training and policy updates keep staff aligned with CMS rules.
Key actions in this step are:
- Monitor KPIs like denial and clean claim rates
- Spot recurring coding or documentation errors
- Update staff on regulatory and payer changes
Common Billing Challenges in Pulmonology and Their Solutions
Pulmonology practices face several specialty-specific billing hurdles that prevent them from getting a consistent income stream. Common challenges include:
- Complex Coding And Policy Changes: Pulmonary diagnostics are diverse, which makes CPT/ICD coding tough for PFTs, sleep studies, and bronchoscopy. Additionally, both payers and AMA frequently update codes and rules, which results in regular denials.
- High Claim Denial Rates: Even small paperwork errors trigger rejections. Industry data show that incomplete documentation or wrong modifiers (e.g., forgetting modifier 25 on a concurrent E/M) are the top denial drivers.
- Payer Authorization and Policy Hurdles: Many pulmonary services (especially sleep studies, advanced imaging, home oxygen) require prior authorization. So when there are delays or denials of authorization, it slows patient care and revenue.
- Equipment and DME Coverage: Billing for devices (CPAP, oxygen, ventilators) is especially tricky and complex. That’s because Medicare and insurers have strict coverage criteria for PAP devices and supplies (documentation of sleep apnea, CPAP titration, etc.).
- Bundling/Modifier Issues: Some pulmonary procedures are bundled, which means they also require modifiers. For example, billing an office visit on the same day as a PFT requires a modifier 25 on the visit. Understanding when to use modifiers 25 or 59 for distinct pulmonary procedures is a common coding challenge.
From these challenges, you can see how they all relate to proper compliance and accurate billing. These challenges reinforce the need for proper billing workflows, where billers stay informed about the regulatory changes.

The Importance of Accurate Coding in Pulmonology
By now, it should be evident that accurate coding is critical in pulmonology. Pulmonary procedures often involve multiple components and rules, so even small coding errors can lead to big revenue losses. Similarly, complex tests like bronchoprovocation or diffusion studies involve multiple CPT codes.
When you use the wrong code or omit a code (e.g., failing to bill for alveolar volume 94727), it can cut payment. Equally, accurate ICD-10 diagnosis coding is needed to justify medical necessity. Conditions like COPD, asthma, sleep apnea, and others have specific codes, and mis-coding these can trigger denials.
All of these things reinstate the importance of accurate coding for pulmonology procedures and how it impacts your revenue. An RCM partner with AAPC-certified coders and billers can offload the billing and coding burden from your practice and ensure error-free claim submissions.
Pulmonology CPT and ICD-10 Billing Codes Cheat Sheet
If your practice is just starting out, a brief sheet containing all the pulmonology ICD-10 and CPT codes can come in handy. Pulmonology billing code cheat sheets help staff quickly find correct codes to avoid claim denials and ensure accurate billing for efficient practice management.
CPT Codes Cheat Sheet for Pulmonary Procedures
Pulmonologists use a variety of CPT codes. Common examples include:
| CPT Code | Description |
|---|---|
| 94010 | Spirometry, lung function test (FVC) |
| 94617 | Cardiopulmonary exercise test (with VO2 max) |
| 94618 | Cardiopulmonary exercise test (per additional 30 min) |
| 94664 | Demonstration/Inhaler or nebulizer training |
| 94640 | Non-invasive ventilation (e.g. CPAP) initiation |
| 31622 | Bronchoscopy, flexible, diagnostic |
| 31625 | Bronchoscopy, rigid, diagnostic |
| 31628 | Bronchoscopy, rigid, with bronchial biopsy |
| 31635 | Bronchoscopy, flexible, with transbronchial biopsy |
| 32555 | Thoracentesis (pleural tap) with imaging guidance |
| 76604 | Ultrasound, chest wall, 1 to 2 views |
| 95806 | Sleep study (PSG), attended in-lab (multi-channel) |
| 95807 | Sleep study (PSG), technician-attended (1 to 4 ch) |
| 95810 | Sleep study (Type II) unattended home test (multi-ch) |
| 94726 | Diffusing capacity (DLCO) single breath |
ICD-10 Codes Cheat Sheet in Pulmonology
These codes are often used for underlying diagnoses in pulmonary claims. For example, Medicare’s pulmonary rehab policy explicitly lists J44.x (COPD) and even the post-COVID code U09.9 as valid reasons for rehab services. Common pulmonary diagnosis codes include:
| ICD-10 Code | Description |
|---|---|
| J44.9 | Chronic obstructive pulmonary disease |
| J45.909 | Asthma, unspecified, uncomplicated |
| J18.9 | Pneumonia, unspecified organism |
| J47.9 | Bronchiectasis, unspecified |
| G47.33 | Obstructive sleep apnea (adult) |
| J42 | Chronic bronchitis, unspecified |
| I27.2 | Other secondary pulmonary hypertension |
| J84.112 | Idiopathic pulmonary fibrosis |
| J84.9 | Interstitial pulmonary disease, unspecified |
| J90 | Pleural effusion |
Important Modifiers in Pulmonology Billing
As explained, modifier 25 must be used “when an E&M code is billed on the same date of service as pulmonary testing codes 94010 – 94799.” This ensures the office visit is paid separately.
Modifier 59 is used when two unrelated procedures occur on the same day. Coding experts must apply these correctly to avoid denials. Pulmonology often uses these key CPT modifiers:
| Modifier | Meaning/Use |
|---|---|
| 25 | Significant E/M on same day as another procedure (e.g. office visit with spirometry) |
| 59 | Distinct procedural service (use when two procedures are separate) |
| 26 | Professional component (physician’s portion of a split service) |
| TC | Technical component (facility/equipment portion of a split service) |
| 95 | Telehealth service via interactive audio/visual technology |
| GT | (Older) Synchronous telemedicine (replaced by 95 for Medicare) |
| XE | Separate encounter (example: separate day, same provider) |
| XS | Separate structure (another anatomical area) |
CMS Updates about Pulmonology Billing
Recently, CMS finalized a new Pulmonology MIPS Value Pathway for 2025. This pathway focuses on quality of care for COPD, asthma, sleep apnea and other lung conditions. Clinicians must now not only code services but also document quality measures (like spirometry for COPD) to earn incentives. This update illustrate how changing rules directly impact billing through new diagnosis codes, covered indications, and reporting requirements.
In 2022, CMS also expanded coverage for pulmonary rehab, as the 2022 Physician Fee Schedule Final Rule added COVID-19-related respiratory rehab to Medicare’s covered conditions. This is especially for patients with persistent respiratory symptoms after COVID. Meanwhile, AMA and payers issue annual code updates.
For instance, new CPT codes or revised ICD-10 codes (such as those for interstitial lung diseases or sleep disorders) are introduced each year. Pulmonologists must adapt to these changes or risk miscoding services. This makes partnering with a knowledgeable billing team even more important. That’s because a specialist can track CMS bulletins, LCDs (Local Coverage Determinations), and payer updates so that your practice remains compliant and reimbursed.
Top Tips to Improve Your Pulmonology RCM
Since your Pulmonology practice’s smooth functionality depends completely on an optimized RCM, here are a few tips to achieve it:
Outsource Pulmonology Billing to a Specialist Team
A dedicated medical billing services provider brings expertise to your revenue cycle. Outsourcing pulmonology billing has been shown to deliver improved accuracy, compliance with regulations, and timely payments. A specialist team is familiar with pulmonary coding intricacies, such as PFT panels, bronchoscopy bundles, etc., and payer rules.
For U.S. pulmonology practices, a company like TransCure, a leading pulmonology billing services provider, acts as that partner. Its trained coders and billers proactively manage claims (with 98%+ first pass rate), appeals, and audits. TransCure’s clients can expect an increased revenue of at least 5 – 10% and A/R delays reduced by 30%.

Create a Pulmonology Billing Codes Cheat Sheet
In the absence of a billing partner, we recommend building an in-house quick reference for your team. List commonly used CPT and ICD codes (as above) and update them annually. Because CPT codes frequently change, this cheat sheet should be a living document.
To make it more helpful, you can include reminders, such as add modifier 25 if E/M + PFT on the same day, to prevent common errors. An important advice here is to regularly review it when new code books or payer policies come out.
Implement a Billing Feedback Loop
The key to ensuring your billing process is going well is to continually monitor performance metrics and adjust. Track key indicators such as claim denial rate, days in A/R, and payment speed. Additionally, regularly pull denial reports to identify common errors, like missing pre-auth and wrong code. After getting this data, use the feedback to train staff and improve processes.
For example, if many claims are denied for missing modifiers, reinforce that rule in team meetings. Industry guidance recommends analyzing denial trends and“monitoring key performance indicators like claim denial rates, reimbursement rates, and time from services to final bill. This loop of measurement and improvement steadily boosts RCM health.
Do Regular Pulmonology Practice Audits
You should conduct periodic audits, even if you are taking services from a third-party billing partner. Check a sample of charts for each provider and verify if documentation supports every code billed. This is an important tip because audits can catch under-billing and over-billing issues early.
Many billing partners, including TransCure, offer complimentary audits before signing up. Auditing ensures that even detailed requirements, like documentation for prolonged ventilator management or pulmonary rehab eligibility, are met. In this way, practices can catch small issues before they become large revenue losses or audit flags.
Frequently Asked Questions (FAQs)
What documentation is required to bill pulmonary rehabilitation under Medicare?
Medicare mandates a physician-prescribed plan of care for pulmonary rehab, reviewed and signed by the doctor every 30 days. Documentation must support chronic lung disease, with notes for each of the 36 sessions over 36 weeks showing medical necessity and required components.
Why do pulmonology claims get denied?
Denials often happen due to coding errors, incomplete documentation, missing pre-authorizations, or incorrectly applying CPT codes and modifiers for specialty procedures. Frequent code updates add extra complexity in preventing denials.
What should you ask when hiring a pulmonology billing company?
Questions should cover collection rates, fee structure, support availability, experience with your specialty, compliance practices, and how quickly they resolve denied claims for better cash flow.
What are common CPT codes in pulmonology?
Some frequently used CPT codes in pulmonology include 94010 for spirometry, 31622 for bronchoscopy, 95810 for sleep studies, and G0424 for pulmonary rehab; correct application ensures proper payment.
Do pulmonary function tests require modifier 25 or modifier 59?
If you see the patient and also do a PFT, bill the E/M with 25. Save modifier 59 for truly unrelated procedures performed in the same session.