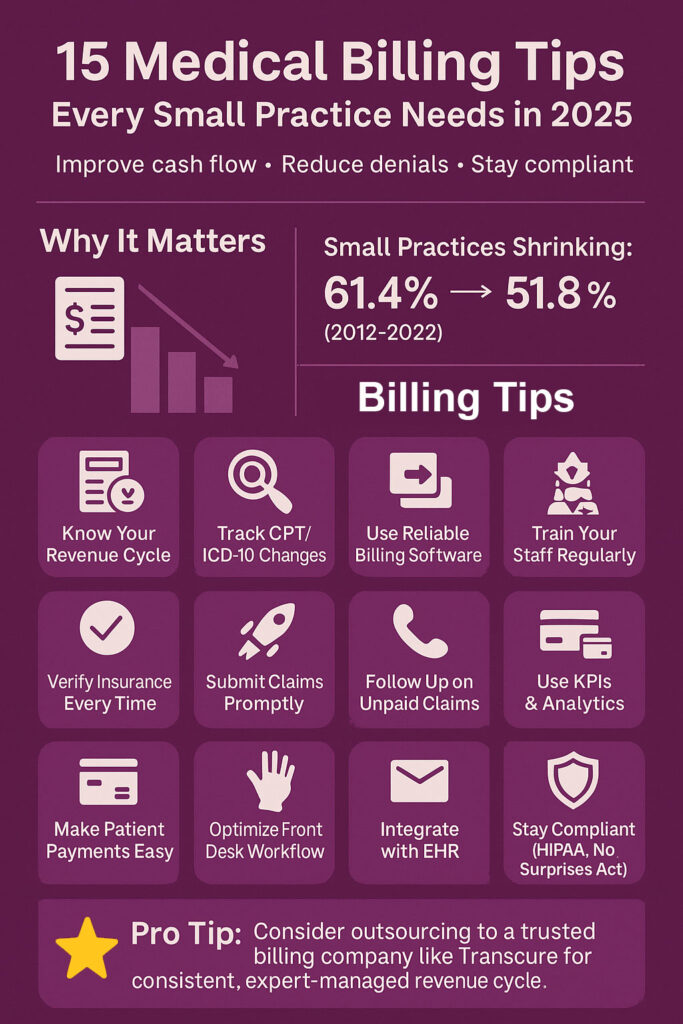
The share of physicians in small practices (10 or fewer physicians) shrank from 61.4 % to 51.8% in U.S. healthcare between 2012 and 2022. This trend underscores the operational and financial challenges faced by smaller practices in the U.S.
Medical billing services for small practices play a critical role in maintaining their financial health amid various operational challenges. Common issues such as coding inaccuracies, claim denials, and delayed reimbursements disrupt revenue inflow, making a small practice unsustainable. Similarly, small practices have limited administrative staff, making it hard for them to manage patient responsibilities and billing work simultaneously.
In this guide, you’ll get 15 expert billing tips explicitly designed for small practices like yours, tips that can help you:
- Cut down on claim denials
- Get paid faster
- Stay compliant
Let’s dive in and fix the medical billing for your small practice.
Get the Best Out of Medical Billing Services for Small Practices (Top 15 Tips)
Tip 1: Understand the Full Revenue Cycle
Medical billing for small practices starts when a patient makes an appointment and continues until the practice receives payment in full. The most important steps are patient registration, insurance verification, documentation of service, coding, submission of claim, posting of payment, and follow-up on accounts receivable.
For small practices, knowledge of each step can help determine where revenue leaks are likely to occur. For example, insurance verification failure causes denials, and delayed coding delays reimbursements.
Tip 2: Stay Updated with CPT and ICD-10 Code Changes
Yearly revisions in CPT and ICD-10 codes may impact billing compliance and accuracy. Inaccurate or obsolete codes usually result in denials or underpayment. Smaller practices should regularly review updates from credible sources like the AMA (for CPT codes) and CMS or CDC (for ICD-10 codes). Getting official newsletters subscribed to or applying software solutions like AAPC Codify or Find-A-Code helps maintain staff updates. Dedicate time per quarter to keep up with updates, particularly those for your specialty. Having current coding knowledge reduces the occurrence of mistakes and aids quicker reimbursements.
Tip 3: Invest in a Reliable Medical Billing Software
Software for medical billing for small practices automates coding, claim submission, denial tracking, and reporting. Search for the following features: automatic coding suggestions, real-time eligibility verification, denial management tools, customizable reporting, and HIPAA compliance. Cloud-based systems are preferred for small practices because of lower initial costs and simple updates. Kareo, DrChrono, and AdvancedMD are some popular ones. They are EHR-integrated and provide patient billing modules. Selecting the appropriate software reduces human errors and enables your staff to concentrate more on patient care.
Tip 4: Outsource When Necessary
Billing services for small businesses may be cost-saving with no in-house expertise. If your denial rate is higher than industry standards (>5%), or claims over 90 days are more than 15%, outsourcing may be worth it. Good medical billing and consulting services provide expert teams, the latest tools, and compliance monitoring. Advantages include increased collection rates, reduced errors, and quicker reimbursement. Companies such as Transcure serve small and mid-sized practices. Review your billing performance statistics prior to making a decision. Outsourcing will pay for itself.

Tip 5: Verify Patient Insurance Before Every Visit
Insurance verification must be done 24–48 hours prior to every appointment. Verify the patient’s coverage, co-pays, deductibles, and service-specific benefits. Perform electronic verification with tools in your practice management system. Automated verification eliminates eligibility-related denials, which contribute up to 25% of all rejections. Train front desk staff to verify information in real-time and resolve issues before the patient checks in. Standardized verification checklist enhances consistency.
Tip 6: Train Staff Regularly
Continuing training keeps your staff current on billing laws, coding changes, and software releases. Concentrate on high-priority topics like ICD-10/CPT coding, denial management, and compliance procedures. Provide quarterly seminars, AAPC or MGMA webinars, or certification assistance like CPC or CPB. Properly trained staff minimize claim errors, enhance collections, and enhance patient satisfaction. Even modest training investments can ward off expensive billing errors.
Tip 7: Reduce Claim Denials Through Accurate Coding
Most claim denials stem from coding errors, such as mismatched diagnosis/procedure codes or omitted modifiers. Use coding audit tools to review charts regularly and correct errors. Implement a double-check system for high-value procedures. Provide coders with specialty-specific coding resources and encourage continuous learning. Just know that denial rates above 5% signal a need for process review. Accurate coding not only reduces rejections but also ensures compliance and optimal reimbursement.
Tip 8: Submit Claims Promptly
Timely claim submission is critical for maintaining cash flow. Aim to submit claims within 24–48 hours of the patient encounter. Delays increase the risk of missing payer deadlines, leading to denied or unpaid claims. Use claim tracking systems in your billing software to flag incomplete submissions. Set automated reminders for daily claim reviews and batch submissions. Speedy submissions reduce your accounts receivable days and accelerate payment cycles.
Tip 9: Follow Up on Unpaid Claims Consistently
Create a structured follow-up schedule to track claims not paid within 30 days. Prioritize high-value claims and aged accounts over 60 days. Use software to categorize and flag claims by denial reason or payer. Standardize follow-up actions: verify status, resubmit with corrections, or appeal with documentation. If a claim remains unresolved after 90 days, escalate to a supervisor or the payer’s dispute resolution team. Consistent follow-up prevents revenue leakage.
Tip 10: Utilize Reporting and Analytics
Monitor your key performance metrics (KPIs) such as days in A/R, first-pass resolution rate, net collection rate, and denial rate. Establish month-to-month goals and trend-watching over periods. Utilize the dashboard capability offered by your billing software. Repetitive reporting reveals inefficiency, so that you can take care of it early on. For example, a sudden spike in denials can point to a coding error or payer policy change.

Tip 11: Improve Patient Payment Collection
Offer multiple payment options, including credit/debit, ACH, and mobile pay. Set clear financial policies and communicate them upfront. Use automated reminders via email/SMS for upcoming and outstanding payments. Implement payment plans for large balances using tools like Rectangle Health or InstaMed. Patient portals also improve transparency and convenience. Effective collection strategies can increase patient payment rates by 30% or more.
Tip 12: Optimize Front Desk Workflow
Efficient front-desk processes reduce billing errors from the start. Use standardized forms for insurance and consent and digital check-in tools to minimize manual entry. Ensure that staff confirm patient demographics and insurance details and collect co-pays at check-in. Create a daily checklist for front desk tasks, including eligibility verification, authorization confirmation, and documentation scanning. Optimizing this first point of contact during the medical billing for small practices improves overall billing accuracy.
Tip 13: Leverage EHR Integration
Connecting your billing program with your electronic health record (EHR) reduces duplicate entries and errors. It ensures coding is pulled directly from clinical documentation, enhancing accuracy. EHR-billing integration helps facilitate quick claim creation and submission for systems that incorporate smooth EHR-billing integration, such as eClinicalWorks, Kareo, or AdvancedMD. Integration cuts billing cycle time by as much as 30%.
Tip 14: Use Clearinghouses to Your Advantage
Clearinghouses act as intermediaries between providers and payers, verifying claims for errors prior to submission. They help lower rejections by identifying faults like invalid codes or missing data. Availity, Change Healthcare, or Office Ally provide real-time claim scrubbing along with status messages. As part of your medical billing services for small practices, utilizing a clearinghouse enhances first-pass claim acceptance rates and shortens reimbursement intervals.
Tip 15: Stay Compliant with HIPAA and Other Regulations
HIPAA compliance helps protect patient information throughout the medical billing process for small practices. You should provide training to your staff on privacy protocols and managing ongoing risk assessment. Keep abreast of federal and state legislation affecting billing activities, such as the No Surprises Act. Non-compliance can lead to fines up to $50,000 per violation, depending on its severity. Utilize HIPAA-compliant software and maintain records of compliance activities to help reduce risk.
Final Thoughts
Medical billing is challenging for small practices. It is hard to escape this process, so it is better to understand its nuances correctly and maintain a healthy cash flow. The above 15 expert tips help your private practice to stay on the right track.Another great option is to outsource medical billing for your small practice to a third-party medical billing company and focus on your patients. One of our recommendations is Transcure for your medical billing services. The company has been in this industry for 12 years and has made a mark with its exceptional medical billing service delivery in multiple states across the U.S.






