Orthopedic practices face unique billing challenges. Complex procedures (like joint replacements, spinal surgeries, or arthroscopies) involve multiple CPT/ICD codes, implants, and long postoperative care. Coordinating diagnostics, surgeries, and follow-up visits is time-consuming, so in-house staff often miss critical details.
Even a single denied claim can cost $25–$100 to resubmit, and repeated denials quickly add up. These oversights not only slow cash flow but can trigger audits and penalties. By outsourcing to a best medical billing company like Transcure, practices can streamline the revenue cycle, cut denials, and stay compliant.

Table of Contents
ToggleWhat Are Orthopedic Medical Billing Services?
Orthopedic medical billing services are end-to-end revenue cycle management for orthopedics. They handle each step of the billing process, which typically includes: insurance verification, patient registration, medical coding (CPT, ICD-10, HCPCS), claim submission, payment posting, denial management, and compliance monitoring.
For example, CPT codes (Current Procedural Terminology) identify surgical procedures (e.g., total knee replacement, CPT 27447). ICD-10 codes record the diagnosis (e.g., M17.12 for knee osteoarthritis). HCPCS codes often cover medical supplies or implants. Accurate coding is critical; in fact, a survey found that coding or data-entry errors cause about 14% of a practice’s lost revenue.
Patient eligibility checks and insurance verification are done first (to confirm coverage and obtain pre-authorizations). Once data is accurate, claims are submitted to payers. When payments arrive, the team posts them and reconciles accounts. Any denials or underpayments are flagged and appealed in denial management. Throughout, compliance with HIPAA and payer rules is enforced. (Notably, federal rules since 2013 require billing partners to have rigorous privacy and breach protocols.) Orthopedic specialists often rely on precise modifier usage and knowledge of global periods (bundled post-op care) to avoid errors. Together, these steps ensure claims are clean and reimbursed promptly.
Key Services Offered in Orthopedic Medical Billing
Orthopedic billing services go beyond generic RCM tasks. Specialist firms offer procedure-specific expertise and targeted support. Key services include:
- Procedure-Specific Coding: Each orthopedic procedure has unique coding rules. Billing experts code surgeries like joint replacements, fracture repairs, or arthroscopies with the proper CPT and modifiers (for example, adding modifier 59 for distinct services). They ensure proper documentation for implants and supplies.
- Global Period Management: Major surgeries (total joint replacements, spinal fusions, ACL repairs) have a 90-day Medicare global period, while minor procedures have 10- or 0-day periods. Billing teams track these periods so all post-op visits are billed correctly. (For example, total knee or hip replacements have a 90-day global window.)
- Prior Authorizations: Many orthopedic surgeries and high-cost devices require insurance authorization. Specialists handle timely PA requests to prevent upfront denials.
- A/R Follow-Up: Dedicated staff chase outstanding claims and patient balances. They monitor aging reports daily and follow up with payers or patients to speed up collections.
- Denial Appeals: When claims are denied (for example, due to coding or documentation issues), the team investigates and resubmits appeals. They use root-cause analysis to reduce recurrence. Specialized knowledge (e.g., modifier rules for repeated injections vs. initial injection) maximizes recovery.
| Procedure Type | Example CPT Code | Global Period | Billing Notes |
|---|---|---|---|
| Major Joint Surgery | 27447 (TKA), 27130 (THA) | 90 days (major) | Includes implant/device coding; bundled rehab visits |
| Arthroscopic Surgery | 29888 (knee scope), 29826 (shoulder) | 10 days (minor) | Post-op visits included: careful with multiple codes |
| Injections / Minor Procedure | 20610 (large joint injection) | 0 days | Procedure visit and injection on the same day; minimal follow-ups |
| Fracture Repair (casting) | 29305 (knee cast) | 90 days (major) | Includes casting on the day of surgery; x-rays are often separate |
These specialized services ensure orthopedic claims, from hip replacements to steroid injections, are coded and processed correctly. By integrating with an EHR (e.g. Epic, Athena) and following the latest CPT/ICD-10 updates, a billing partner prevents common errors before they happen.
6 Business Benefits of Outsourcing Orthopedic Billing
Outsourcing orthopedic billing can dramatically improve a practice’s financial health. Key benefits include:
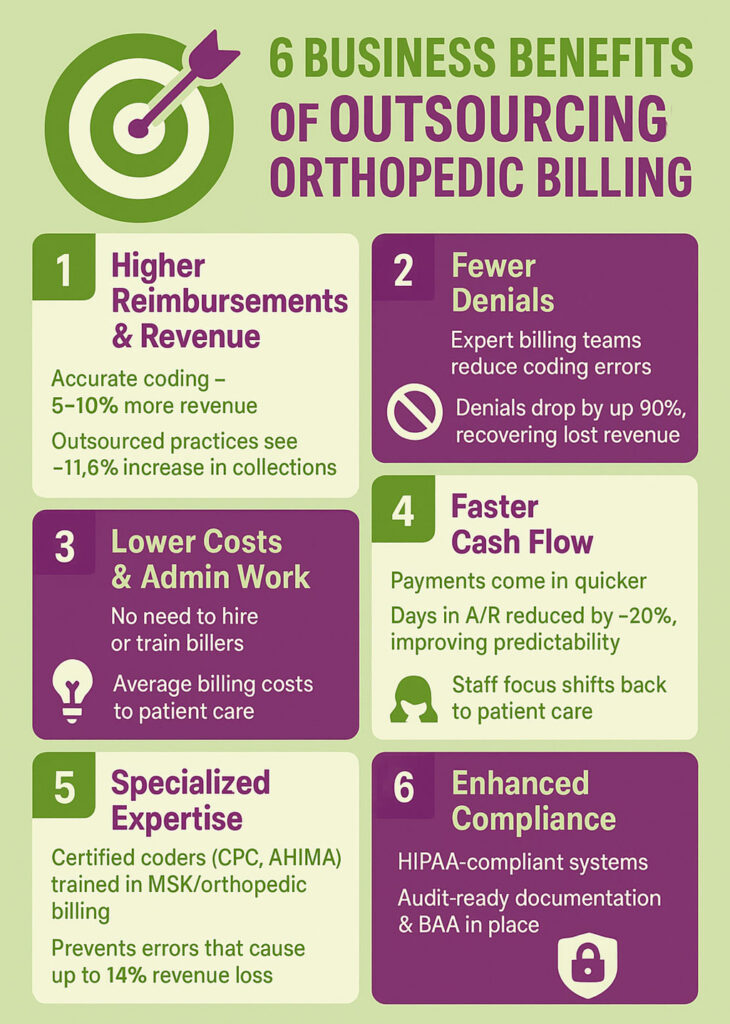
1. Higher Reimbursements & Revenue: Specialist coders optimize every claim. Accurate coding can boost revenue by 5–10%. In fact, practices that outsource see an average revenue increase of about 11.6%. (If you’re looking to improve payment cycles and collections further, check out our guide on how to get paid for orthopedic services.)
2. Fewer Denials: Expert teams prevent common coding mistakes (like wrong modifiers or missing documentation). Studies show outsourcing denial management can cut denials by ~90%. With denied claims under control, practices recover thousands that would otherwise be written off.
3. Faster Cash Flow: Outsourced billing accelerates payments by streamlining processes. One industry report found a 20% reduction in days in accounts receivable with outsourcing. Faster collections mean more predictable cash flow for your practice.
4. Lower Costs & Administration: Outsourcing eliminates the need to hire and train in-house billers. Practices typically reduce their billing costs (~16.9% lower expense on average) and avoid overhead like software licenses. Freed staff can focus on patient care or other tasks.
5. Specialized Expertise: Orthopedic billing partners employ certified coders (CPC/AHIMA) who train specifically on MSK procedures. They stay current on coding changes and payer rules. This expertise prevents costly errors (nearly 14% of revenue loss stems from coding mistakes) and ensures best-in-class RCM.
6. Enhanced Compliance: Outsourced firms build strict compliance into their workflow. They maintain HIPAA-compliant policies, clear Business Associate Agreements, and audit-ready documentation. This reduces the risk of fines or breaches. With experts on hand, you can rest assured that you meet evolving regulatory requirements.
Overall, outsourcing medical billing for orthopedics provides a strong ROI. Reduced denials and administrative costs pay for the service many times over, while improved collections flow directly to your bottom line.
Signs You Need an Orthopedic Billing Partner
Watch for these red flags, which often indicate it’s time to outsource:
- Frequent Claim Denials: If denial rates are climbing (MGMA found 60% of practices saw higher denials year-over-year) and many claims aren’t even appealed (up to 50–60% are never worked), you’re losing revenue.
- Growing Accounts Receivable (A/R): Prolonged days in A/R (over 60+ days) or a large A/R backlog means money is tied up. Specialist billers use aggressive follow-up to shrink A/R quickly.
- Small or Overloaded Billing Staff: If your team is swamped or you only have 1–2 billers, complex orthopedic cases may be falling through the cracks. A partner can scale with your volume.
- Modifier/Compliance Confusion: Constant write-offs due to modifier mistakes (MGMA reports “incorrect modifier usage” as a top denial cause) or lack of knowledge of global periods suggest you need expertise.
- Audit Risk & Compliance Gaps: Frequent payer audits or worry over HIPAA means the billing workflow may not be fully compliant. Experts proactively manage audit responses and regulatory changes.
- Rising Costs with Diminishing Returns: If you’re investing more in billing (new software, overtime) but collections aren’t improving, outsourcing efficiency will benefit you.
If you recognize these pain points in your practice, it’s time to consider a professional orthopedic billing partner.
How to Choose the Right Orthopedic Billing Partner
When selecting a partner, evaluate these criteria:
- Orthopedic Specialization: Look for a provider with proven experience in orthopedics. They should understand joint replacement coding, spinal surgeries, sports medicine procedures, etc. Verify they have references from other orthopedic clients.
- Certified, Trained Staff: Ensure their coders and billers are certified (CPC, CCS-P, etc.) and receive ongoing education. Confirm they attend workshops and track CMS coding updates. A knowledgeable team avoids “lost revenue nightmares.”
- Transparent Reporting: The partner should offer clear dashboards and regular reports on key metrics (collections, A/R aging, denial rates, etc.). Transparency builds trust and helps you track ROI.
- EHR/PM Integration: They must work with your practice management system or EHR. Check if they have experience with your software (e.g. Epic, Cerner, Athena). Seamless data flow prevents entry errors.
- Proven Track Record: Ask about case studies or client outcomes. Have other orthopedic customers seen improvements? (For example, Transcure often highlights 20%+ revenue gains or faster payment cycles.)
- Compliance and Security: Verify they provide a Business Associate Agreement (BAA) and follow HIPAA Omnibus Rule standards. They should have strict data security and breach protocols.
- Customer Support: Good billing firms treat you as a partner. Confirm they have responsive support, such as dedicated account managers or 24/7 access.
Ultimately, trust your instincts. A good partner listens to your needs, asks detailed questions about your practice, and crafts a customized approach.

Final Thoughts: Why Transcure Is a Smart Choice
Outsourcing orthopedic billing unlocks more revenue and less stress. By partnering with experts, your practice avoids costly coding errors, slashes denial write-offs, and accelerates cash flow. Transcure specializes in orthopedic revenue cycle management and offers proven processes, certified coders, and seamless EHR integration. Our clients consistently see significant gains in collections and efficiency.
Don’t let billing errors or denials hold your practice back. Partner with Transcure and experience accurate, efficient, and compliant orthopedic medical billing.
Frequently Asked Questions (FAQs)
What makes orthopedic billing different?
Orthopedic billing involves a mix of surgeries, follow-up care, and durable equipment. Procedures often have global payment periods and use specific CPT modifiers. For instance, total knee replacements carry a 90-day post-op bundle, and injection services may require modifier 59 when done on the same day as other procedures. Implants (like artificial joints) use HCPCS supply codes.
This complexity, handling multiple procedure codes, tracking follow-ups, and securing authorizations for implants, sets orthopedic billing apart. A specialized billing team understands these nuances and ensures each step is documented to avoid denials.
How do outsourced services reduce denials?
Billing experts reduce denials through accurate coding and proactive follow-up. They verify insurance and obtain prior authorizations before procedures, so claims aren’t rejected for eligibility issues. Expert coders apply the correct CPT/ICD codes and modifiers, preventing common errors (for example, MGMA notes incorrect modifiers as a frequent reason for denial).
If a claim is denied, dedicated staff quickly investigate, appeal, or rebill it correctly. Studies show specialized denial management can cut denials by ~90%. By catching issues early and addressing them systematically, outsourced teams dramatically improve clean-claim rates and cash collections.
What information does a billing company need to get started?
To begin, an orthopedic billing partner will need your practice demographics (NPI, tax ID, location), provider credentials, and fee schedules. They’ll ask for payer information (a list of insurance contracts/fee schedules) and an EHR or practice management login for data access. Often, you’ll share a BAA for HIPAA compliance. Providing historical billing data (old claims reports, remittance advice, A/R aging) helps them identify trends.
The more information you give, from patient demographics to documentation standards, the faster and more accurately they can set up your account. Transcure, for example, works closely with practices to configure workflows and verify credentials before going live, ensuring a smooth transition.