Cancer care usually involves expensive drugs, frequent treatments, and highly specialized procedures. Every step, from prior authorization to claim submission, can impact how quickly practices receive payment and how smoothly patients receive care.
An ASTRO survey reports that oncology physicians handle about 39 prior authorization requests weekly, consuming 13+ staff hours. Billing for chemotherapy and specialty drugs further complicates the process. Nearly 30% of oncology claims face initial denials, forcing practices to spend additional time on appeals and corrections, straining revenue.
This 2026 guide explains what oncology medical billing really is in detail. From the most common challenges practices face to the essential codes you need to know, we will go through every aspect. The goal is to help practices simplify workflows and reduce denials to strengthen cash flow in an increasingly complex oncology medical billing service.

Table of Contents
Toggle- Why Medical Billing for Oncology is Unique: Key Components and Challenges
- The Step-by-Step Process of Oncology Medical Billing
- Oncology Billing Made Simple with the Oncology Coding Cheat Sheet 2026
- Must Follow Oncology Billing Guidelines for 2026
- Medical Billing for Oncology Tips and Tricks for 2026
- Final Thoughts
- FAQs on Oncology Medical Billing
Why Medical Billing for Oncology is Unique: Key Components and Challenges
Oncology billing stands out because every patient visit involves multiple services, high-cost drugs, and strict insurance rules. So, let’s look at the main components that make coding and claim submission more complex in medical billing for oncology:
1. Medical vs. Radiation Oncology Billing
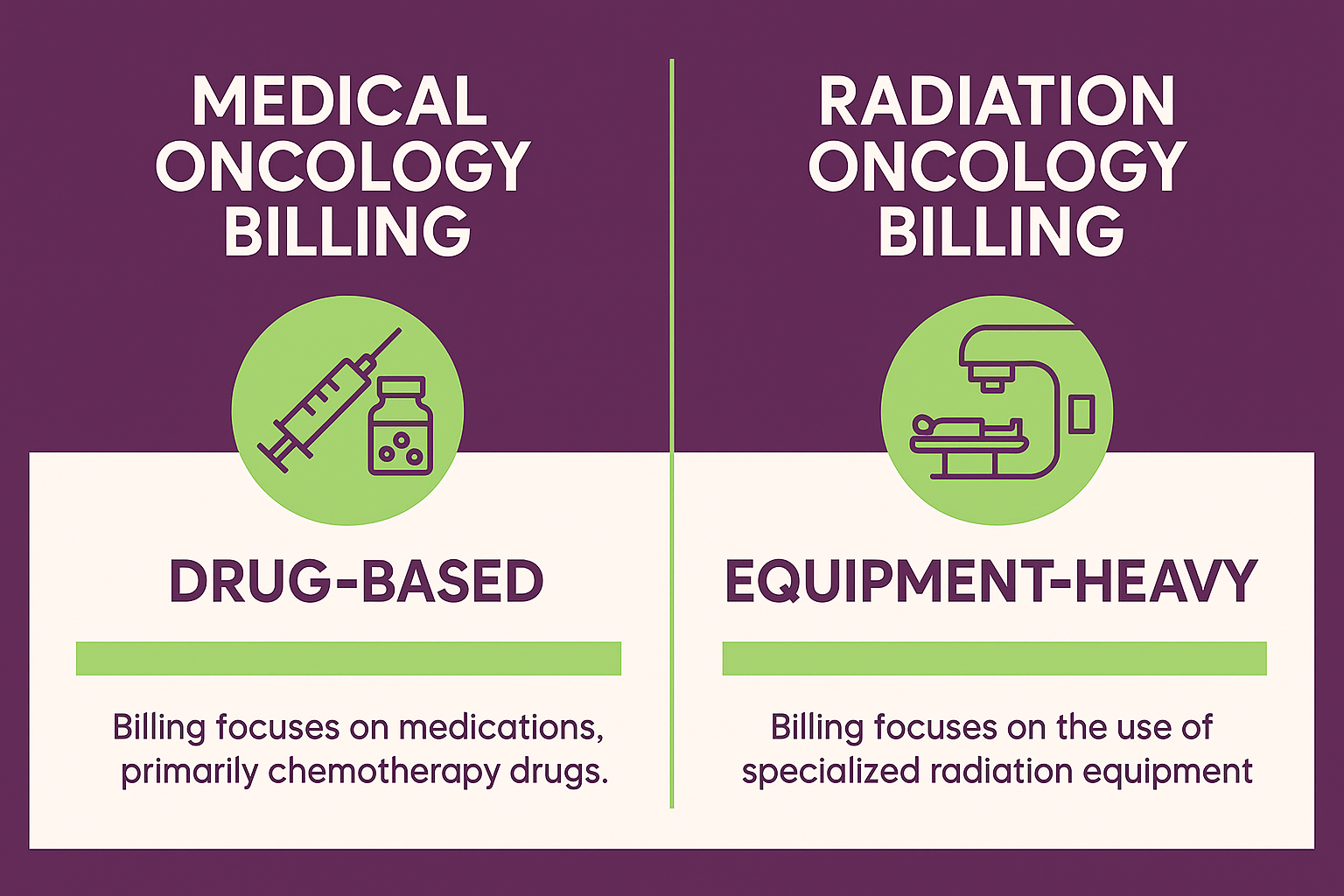
Medical Oncology Billing: It focuses on drug-related care such as chemotherapy, biologics, and immunotherapies. This part also includes follow-up visits and supportive treatments.
Radiation Oncology Billing: This involves both physician services and technical use of equipment. Each radiation session often requires several codes, making accuracy essential.
2. Prior Authorizations in Oncology
Prior authorizations are most important in oncology. Chemotherapy, biologics, and immunotherapies almost always need approval before treatment. Any delay or missing detail can cause denials, slowing down both patient care and payment.
3. Bundled Billing Guidelines
Payers often apply oncology billing guidelines that bundle services like infusion and drug administration. Without proper modifiers and documentation, practices risk receiving less than what they are owed. This is also a core reason why oncology claims face higher denial rates than most specialties
4. Compliance and Accuracy
Because of the high cost of cancer care, insurers closely monitor claims. Even a minor error in oncology CPT codes can lead to revenue loss or compliance audits. Many practices reduce risks by working with an oncology medical billing company or using detailed internal reviews.

The Step-by-Step Process of Oncology Medical Billing
Oncology medical billing follows a structured process from the moment a patient registers until the balance is cleared. Each step requires accuracy to prevent delays or denials. Below is the full cycle of how medical billing for oncology typically works:
1. Patient Registration and Insurance Verification
The first step is gathering patient demographics and insurance details. Staff must verify eligibility for oncology services, including chemotherapy, radiation, and biologic therapies. Errors at this stage can lead to denied claims, so accuracy is critical.
Many patients also carry secondary insurance. Identifying it early ensures proper coordination of benefits and prevents surprise bills. Practices should also explain financial responsibility upfront so patients know their share of costs before treatment begins.
2. Prior Authorization and Clinical Documentation
High-cost drugs and radiation therapies almost always require prior authorization. Staff must submit requests with diagnosis details, treatment staging, and projected therapy plans. Missing authorizations can stop care or create full denials, which impact both patients and revenue cycles.
Clinical documentation strengthens the approval process. Oncologists and nurses must note the prescribed drugs, infusion times, and patient responses. Complete records not only support authorization but also help meet oncology billing guidelines for compliance.
3. Medical Coding and Charge Entry
Accurate coding is the backbone of medical oncology billing. Coders assign ICD-10 codes for diagnoses and CPT/HCPCS codes for chemotherapy, infusions, and radiation services. Modifiers and drug units must reflect exactly what was delivered to avoid underpayment.
Once coded, charges are entered into the billing system. Here, clean data capture ensures claims reflect the full scope of care. This also means practices need to stay updated on new and revised codes.
4. Claim Preparation and Submission
Claims move through a scrubber tool to catch missing details or errors. This step reduces rejections and increases the first-pass acceptance rate. Clean claims are then submitted electronically through a clearinghouse for faster payer review.
Staff should track rejections immediately. Correcting issues before resubmission prevents delays. Electronic claim submission is now the standard in oncology medical billing, as it speeds up processing and ensures greater transparency in claim tracking.

5. Payer Adjudication and Denial Management
Insurance companies review claims during adjudication. They either approve payment, reduce it, or issue denials. The Explanation of Benefits (EOB) outlines why a claim was adjusted or rejected.
Denial management is vital in oncology billing and coding. Staff analyze denial trends, correct errors, and file appeals with strong documentation. Quick appeals can recover significant revenue, as up to 79% of denials are reversed on appeal.
6. Patient Billing and Collections
After payer processing, patients receive statements for deductibles, co-pays, or non-covered services. Transparent statements improve patient trust and reduce confusion about what they owe.
For high balances, practices often set up flexible payment plans. This approach increases collection rates while keeping care accessible to patients facing the high costs of cancer treatment.
Oncology Billing Made Simple with the Oncology Coding Cheat Sheet 2026
Oncology medical billing depends on precise coding at every step. As even small errors can cause denials or payment delays, the following is an oncology coding cheat sheet 2026 for practices:
1. ICD-10 Diagnosis Codes
ICD-10 codes identify the type and location of cancer for billing and insurance purposes. Accurate coding is essential in medical oncology billing because payers use these codes to justify treatments like chemotherapy, biologics, and radiation therapy.
| Category | ICD-10 Code | Description |
|---|---|---|
| Malignant neoplasm of breast | C50.xx | Codes vary by breast quadrant and laterality |
| Malignant neoplasm of prostate | C61 | Prostate cancer |
| Malignant neoplasm of lung | C34.xx | Codes specify lung lobe and side |
| Malignant neoplasm of colon | C18.xx | Codes specify colon segment |
| Malignant neoplasm of rectum | C20 | Rectal cancer |
| Malignant neoplasm of pancreas | C25.xx | Codes vary by part of pancreas |
| Secondary malignant neoplasm | C77–C79 | Metastatic cancers (lymph nodes, bone, brain, etc.) |
| Leukemia | C91–C95 | Includes lymphoid, myeloid, monocytic types |
| Lymphoma | C81–C86 | Hodgkin and non-Hodgkin lymphomas |
| Malignant neoplasm, unspecified | C80.1 | Cancer, unspecified primary site |
2. CPT Procedure Codes
CPT codes describe the actual services provided during cancer treatment. In oncology medical billing, their correct use ensures providers receive proper reimbursement for chemotherapy, infusions, and patient visits.
Chemotherapy Administration Codes
These codes cover the administration of chemotherapy and other anti-cancer agents. They vary by delivery method and duration.
| CPT Code | Description |
|---|---|
| 96401 | Chemotherapy, subcutaneous or intramuscular, single drug |
| 96402 | Hormonal antineoplastic injection |
| 96409 | Chemotherapy IV push, single drug |
| 96411 | IV push, each additional drug |
| 96413 | Chemotherapy IV infusion, up to 1 hour, single drug |
| 96415 | Each additional hour of infusion |
Infusion and Injection Codes
These codes apply to non-chemotherapy infusions such as hydration, biologics, and supportive medications.
| CPT Code | Description |
|---|---|
| 96360 | IV hydration, initial 31 minutes–1 hour |
| 96361 | IV hydration, each additional hour |
| 96365 | IV infusion, therapeutic/prophylactic, up to 1 hour |
| 96366 | Each additional hour of infusion |
| 96367 | Additional sequential infusion, new drug/substance |
| 96372 | Therapeutic or prophylactic injection, subcutaneous or intramuscular |
Evaluation & Management (E/M) Codes
E/M codes capture patient visits for counseling, care coordination, and follow-up. They are commonly billed with oncology treatments.
| CPT Code | Description |
|---|---|
| 99213 | Established patient, office visit, low–moderate complexity |
| 99214 | Established patient, office visit, moderate complexity |
| 99215 | Established patient, office visit, high complexity |
| 99203 | New patient, office visit, low–moderate complexity |
| 99204 | New patient, office visit, moderate complexity |
| 99205 | New patient, office visit, high complexity |
3. HCPCS Drug and Supply Codes
HCPCS codes capture the drugs and supplies used during oncology treatments. These codes are essential for billing chemotherapy, biologics, immunotherapies, and supportive medications. Each code corresponds to a specific drug formulation and dosage unit.
| HCPCS Code | Drug / Supply | Description |
|---|---|---|
| J9000 | Doxorubicin HCl | 10 mg injection |
| J9190 | Fluorouracil | 500 mg injection |
| J9312 | Rituximab | 10 mg injection |
| J9355 | Trastuzumab | 10 mg injection |
| J1100 | Dexamethasone sodium phosphate | 1 mg injection |
| J7030 | Normal saline | 1,000 mL infusion |
| J7050 | Normal saline | 250 mL infusion |
| A4216 | Sterile water/saline | Per 10 mL |
| A4221 | Supplies for chemotherapy infusion, pump | Each |
Must Follow Oncology Billing Guidelines for 2026
Oncology billing rules change often, and payers set strict requirements for cancer treatments. Following updated oncology billing guidelines helps practices reduce denials and protect revenue. Below are the key areas every oncology team must focus on.
1. Compliance with CMS and Payer Requirements
Oncology medical billing must follow rules set by CMS (Centers for Medicare & Medicaid Services) and private insurers. These rules define how chemotherapy, infusion, and radiation services should be documented, coded, and billed. The failure to meet them can lead to audits, penalties, or payment delays.
Every payer may have unique rules for prior authorizations, modifiers, or bundled services. Billing teams should review payer updates regularly and cross-check claims before submission. Staying compliant protects practices from denials and ensures accurate reimbursement for high-cost oncology care.

2. Documentation Best Practices
Accurate documentation is the backbone of medical oncology billing. Each patient record should clearly state the diagnosis, treatment stage, drug details, infusion times, and patient response. Missing or vague notes often lead to denied claims or underpayment.
Providers and nursing staff should record information in real time. Best practices include using standardized templates, listing exact drug units, and attaching prior authorization approvals. Complete documentation supports payment and ensures compliance with the latest oncology billing guidelines.
3. Avoiding Common Billing Errors
Billing mistakes are a leading cause of denied oncology claims. Errors usually include incorrect oncology CPT codes, missing modifiers, or using outdated HCPCS drug codes. Even small mistakes can cost thousands of dollars in lost revenue.
To avoid these issues, billing teams should double-check drug units, verify prior authorizations, and use claim scrubbers before submission. Regular staff training and reference tools, or outsourcing to an oncology medical billing company like Transcure, also help reduce errors and speed up reimbursement.
Medical Billing for Oncology Tips and Tricks for 2026
Oncology billing can be overwhelming, but small improvements make a big difference in revenue and efficiency. The following medical billing tips and tricks help practices streamline processes, cut denials, and keep cash flow steady:
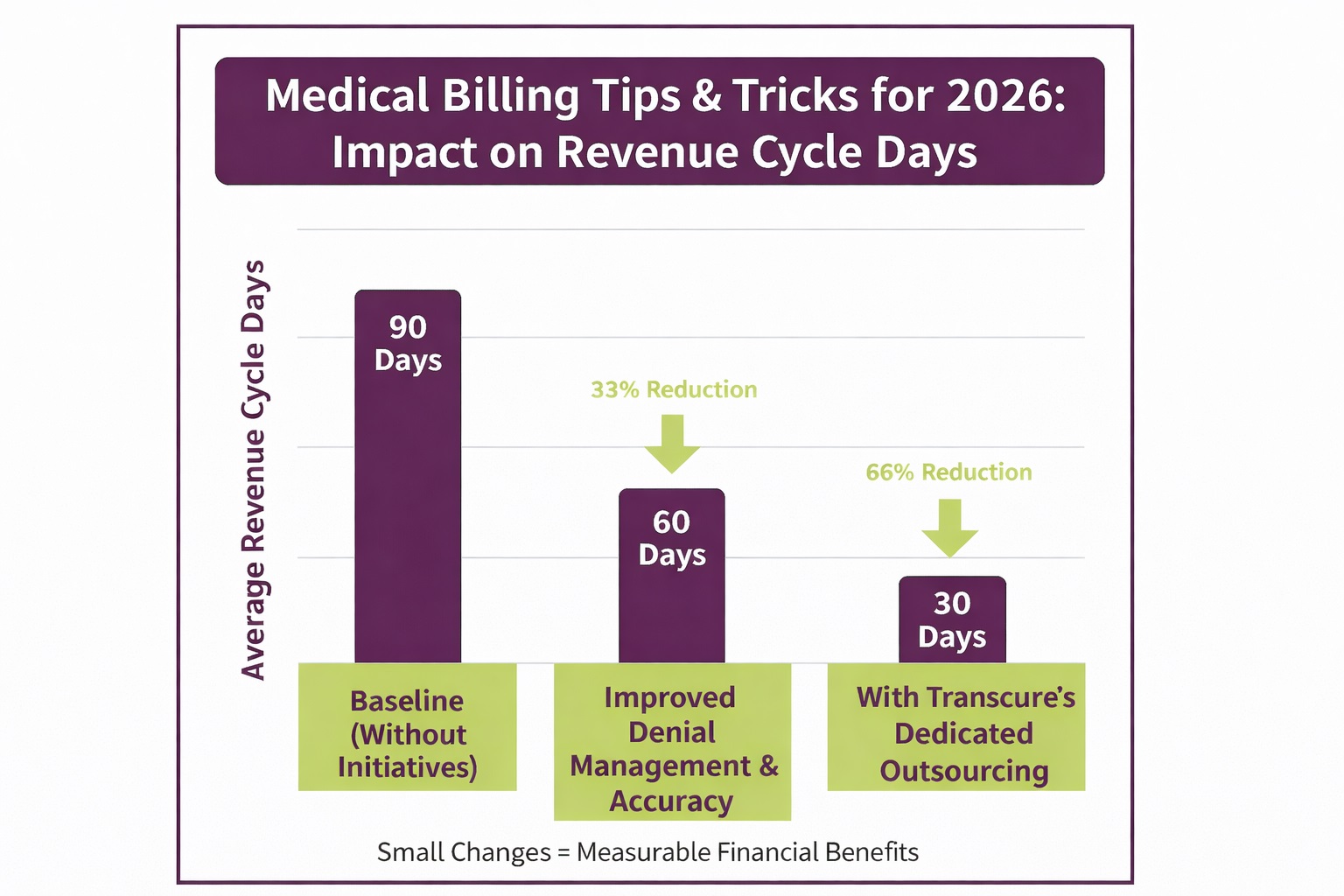
1. Denial Management and Appeals
Claim denials are common in oncology because of prior authorization errors, incomplete documentation, or incorrect oncology CPT codes. Every denied claim means delayed revenue and extra staff workload. So, successful practices build a system to track, analyze, and quickly resolve denials.
A strong appeals process includes reviewing payer denial patterns and correcting errors. Then, resubmit them with supporting documents like clinical notes and authorizations. Many practices also partner with specialized billing teams such as Transcure, whose oncology denial management strategies have helped practices cut A/R days to near 30.

2. Maximizing Revenue with Accurate Coding
Accurate coding is one of the most effective ways to protect oncology practice revenue. Using the correct ICD-10 and CPT procedure codes ensures payers recognize every service delivered, from chemotherapy infusions to radiation therapy. Even small coding errors can cause underpayments or outright denials.
To avoid these losses, billing teams should use coding references, stay updated with changes, and apply modifiers properly. Some practices also rely on experts like Transcure, whose oncology billing specialists provide infusion coding and ICD-10 staging documentation. Their payer-specific coverage knowledge helps practices capture their full reimbursement potential
3. Leveraging Technology and AI in Billing
Technology now plays a major role in medical billing for oncology. Tools like automated eligibility checks, claim scrubbers, and AI-driven coding assistants help reduce manual errors and speed up claim submission. This means faster reimbursements and fewer denials.
Advanced solutions such as Robotic Process Automation (RPA) can handle repetitive billing tasks like charge entry and claim tracking. Many oncology practices turn to partners like Transcure, which integrates automation and AI into billing workflows. This gives providers real-time reporting and reduces overall costs by a lot.
Final Thoughts
Oncology medical billing in 2026 demands accuracy, compliance, and efficient workflows. From prior authorizations to coding and denial management, every step impacts how quickly practices are paid and how smoothly patients receive care. Small improvements can make a major difference in revenue stability.
Many practices choose to work with specialized billing partners like Transcure, a trusted oncology medical billing company with decades of experience. By combining expertise and automation with payer rules, Transcure helps practices reduce denials and improve collections.
FAQs on Oncology Medical Billing
What is the difference between global and split billing in oncology?
Global billing covers both the professional and technical components of a service, such as radiation therapy. Split billing separates these parts, with one claim for the physician and another for the facility.
How do oncology practices handle clinical trial billing?
Routine care costs in clinical trials are billed to insurance, while trial-related services are billed to the sponsor. Clear documentation is key to avoiding billing patients for services that should not be charged.
Why is drug waste reporting important in oncology billing?
Payers like Medicare require providers to bill for wasted amounts of single-use vials. Reporting drug waste with the correct modifiers ensures compliance and allows practices to recover the cost of unused medication.
What role do National Drug Codes (NDCs) play in oncology billing?
NDCs identify the exact drug, strength, and packaging. Including NDC numbers on claims helps payers verify the medication used and prevents claim rejections for chemotherapy and biologics.
How often should oncology billing teams update their coding knowledge?
Oncology codes change frequently, especially for new drugs and therapies. Billing staff should review quarterly payer updates and annual CMS changes to stay compliant and avoid costly mistakes.









