According to the KFF 2023 report, U.S insurers processed approximately 425 million claims, out of which 73 million were denied. This reflects a denial rate of 19%, causing serious revenue delays that can last up to 30-120 days. Recovering these payments afterward becomes a tricky and complex process. To tackle this growing challenge, healthcare providers should consider seeking assistance from outsourced revenue cycle management companies.
Revenue cycle companies handle every aspect from insurance verification to collecting final reimbursements, to ensure your revenue flows smoothly. With so many companies offering RCM solutions, finding the perfect fit for your practice is important. If you’re new to the healthcare industry in the U.S, this article will be your guide to discovering the top revenue cycle management companies.
Table of Contents
ToggleTop 10 Revenue Cycle Management Companies in USA
The following is the list of the top Revenue Cycle Management Companies in USA in 2025:
- Transcure
- Athenahealth
- CureMD
- Access Healthcare
- eClinicalWorks
- R1 RCM
- CorroHealth
- GeBBS Healthcare Solutions
- CareCloud
- Trizetto
Let’s now explore each revenue cycle management company in detail, and let’s find out which one is the best for your practice.
1- Transcure

Transcure is one of the leading revenue cycle management companies in USA, delivering personalized revenue cycle management services specially designed for hospitals, clinics, and solo medical practices. With a strong track record and over 500 satisfied physicians, Transcure delivers end-to-end billing solutions according to the unique needs of practitioners.
Moreover, they provide complete RCM services for over 44 specialties, including cardiology, podiatry, and more. One key feature that sets Transcure apart from its competitors is its up to 98% first-pass clean-claim rate, which speeds up the reimbursement collection.
Other than that, Transcure has 1100+ certified medical billers and coders who ensure accurate coding and full compliance with the industry regulations. In addition, this top RCM company conducts proactive A/R follow-ups to help practices maintain a steady cash flow by promptly addressing previous unpaid claims.
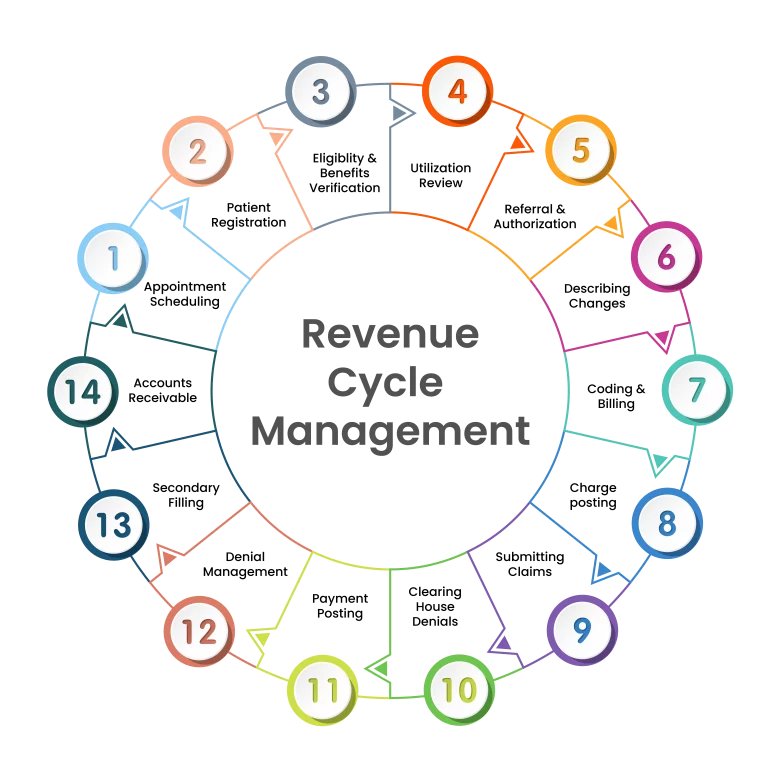
Moreover, Transcure has created a comprehensive guide detailing the 14 steps of revenue cycle management for your convenience. By reading it, you’ll gain a clear understanding of the RCM cycle and identify stages where professional assistance by RCM companies may be needed.
Its Key Offerings Include
- End-To-End RCM Services: Offers a complete suite of RCM services, including appointment scheduling and patient registration to charge posting, coding, payment processing, denials management, and patient collections.
- Compatibility with Major EHRs: RCM solutions are fully compatible with all major EHR systems like Epic, Athenahealth, and others.
- Compliance-Backed Operations: They are certified with ISO 27001, AICPA SOC 2, and HIPAA to ensure data security.
- Robotic System Automation: RPA-powered coding process ensures 99% accurate claim submissions.
- Free Credentialing Service: Transcure provides cost-free credentialing services to all providers who choose our RCM package for their preferred payor network.
- Complimentary Old A/R Recovery: Along with the RCM suite, Transcure offers free AR recovery services and shows up to a 30% reduction in outstanding accounts receivable.
Why Transcure Must be Your First Choice?
- 48 Hours Turnaround Time: This healthcare RCM company ensures a rapid turnaround time, with denial resubmissions processed within just 48 hours.
- 5%-10% Revenue Growth: Their efficient claims management and follow-ups enable a revenue growth of 5%-10% for their clients.
- 30% Reduction in A/R: Transcure reduces accounts receivable by 30% and shortens A/R days to 24 days.
- 99% Customer Retention Rate: They maintain a 99% customer retention rate that shows strong client satisfaction and loyalty.

2- Athenahealth

Athenahealth is one of the best RCM companies formed in 2019 through the merger of two companies athenahealth, Inc. and Virence Health. With a powerful combination of revenue cycle management, clinical records, and patient engagement services, Athenahealth streamlines healthcare operations for providers across the country.
The platform’s low-touch approach uses powerful automation tools to handle routine A/R follow-up tasks independently that reduces the administrative burden in a practice. Moreover, Athenahealth is compatible with all major EHRs, so RCM upgrades can be implemented seamlessly without the need to change your existing EHR system.
Its Key Offerings Include
- Integrated clearinghouse services
- RCM services for 30+ medical specialties
- Claim resubmission
- Denial management
3- CureMD

CureMD is a leading healthcare technology company in the USA, providing personalized revenue cycle management (RCM) solutions for hospitals, clinics, and solo practices. Their services streamline the entire billing process — from patient registration and eligibility verification to coding, claim submission, denial management, and payment posting.
CureMD supports over 40 specialties and combines certified medical billers and coders with AI‑driven automation to ensure high clean-claim rates, faster reimbursements, and full compliance with HIPAA standards.
Its Key Offerings Include
- Comprehensive management of the revenue cycle, including A/R follow-ups and patient collections.
- Works seamlessly with CureMD’s EHR and other major systems.
- AI-enhanced coding and claim validation for faster, error-free submissions.
- Advanced reporting and analytics to monitor collections, denials, and financial performance.
- HIPAA-compliant operations to protect patient and financial data.
CureMD helps practices maximize revenue, reduce A/R days, and focus on delivering quality care without administrative burdens.
4- Access Healthcare

Access Healthcare stands out as a technology-driven RCM partner with a team of 27,000 revenue cycle professionals dedicated to deliver end-to-end RCM services. They manage patient scheduling, eligibility verification, prior authorizations, and accurate patient registration to reduce claim denials.
Moving into mid-revenue cycle services, Access Healthcare oversees charge entry and conducts charge audits to maintain billing accuracy and quick claim submission.
Their certified medical coders assign the correct procedure and diagnosis codes to improve reimbursement rates and minimize denials. On the back-end, the accounts receivable management team actively follows up on outstanding payments and collections to maintain steady cash flow.
Its Key Offerings Include
- Medical coding audit
- Resolves denied claims
- Certified medical billing specialists
- Robotic RCM automation platform
5- eClinicalWorks
eClinicalWorks provides both self-service RCM technology and fully managed end-to-end RCM services. With a customer base of more than 850,000 medical professionals worldwide, this revenue cycle management company has become a trusted partner for healthcare practices. Their AI-powered platform handles appeals, coding, eligibility checks, billing, and patient collections while reducing manual error.
Moreover, eClinicalWorks even employs AI bots to clean and submit claims to insurance companies. The platform also supports automated electronic remittance posting and provides tools for effective denial and appeal management. To help practices stay ahead of payer deadlines, they have also developed an Alerts Dashboard that highlights priority claims.
Its Key Offerings Include
- Work queue dashboards
- AHIMA/ AAPC certified coding experts
- Performance evaluation tools
- Daily, monthly, and year-to-date statements and reports

6- R1 RCM

R1 RCM offers comprehensive revenue cycle services to various healthcare organizations, from hospitals to physician practices. Their services include scheduling, registration, Coding, billing, and collections, so it’s a one-stop shop for enterprises with high operational demands. To ensure accuracy, they utilize Palantir-powered AI technology that helps reduce denials and optimize reimbursements.
R1 also integrates self-service options, such as online scheduling, automated payment plans, and omnichannel support that make billing more convenient. On top of that, they even offer A/R recovery services that help practices to achieve a 20% increase in patient collections.
Its Key Offerings Include
- Claim follow-up
- Advanced analytics for performance optimization
- Charge capture tool
- Advanced coding management
7- CorroHealth

CorroHealth is a leading U.S.-based RCM company that delivers technology-enabled solutions to healthcare providers and payers. It offers a complete suite of RCM services, ranging from patient registration and eligibility verification to coding and claim submission. Since billing is a critical step in the RCM cycle, CorroHealth ensures accuracy by using AI-powered automation to deliver precise medical coding.
Furthermore, to reduce the risk of claim denials from the insurance companies, they perform claim edits and conduct pre-submission reviews. CorroHealth also offers AR management and follow-up services to help healthcare providers collect payments faster by working closely with insurance companies.
Its Key Offerings Include
- 3,000 experienced and specialized coders
- Payment posting & reconciliation
- Real-time payment tracking and reporting
- Tailored workshops and training
8- GeBBS Healthcare Solutions

GeBBS Healthcare Solutions is also among the top 10 healthcare revenue cycle management companies in usa with 10–15 years of expertise in the RCM industry. They offer comprehensive medical revenue cycle management services tailored for small to mid-sized practices. Their cost-effective services make this company an ideal choice for providers with limited budgets.
This healthcare RCM company is mainly known for its focus on coding accuracy and denial management. With a team of certified coders who are skilled in CPT and ICD-10 codes, this company helps practices reduce claim errors and accelerate reimbursements. Also, GeBBS’s advanced technology platforms, such as iCode Assurance, provide comprehensive coding audits and real-time quality checks.
Its Key Offerings Include
- AI-driven RCM services
- Eligibility and prior authorization verification
- Cloud-based AR automation
- Detailed metrics and reporting
9- CareCloud

CareCloud is one of the best medical revenue cycle management companies, currently operating in 50 states in the U.S. They offer AI-powered RCM services to small clinics, large medical groups, and complex health systems through a cloud-based, all-in-one platform. CareCloud offers support for the complete revenue cycle from patient registration to payment collection by automating tasks.
This RCM company is integrated with major EHR platforms, which eliminates the need for providers to switch their existing systems. Additionally, CareCloud offers real-time performance analytics to let practitioners monitor their financial performance and track revenue.
Its Key Offerings Include
- Denial prevention tools
- Appeals automation
- HIPAA compliance services
- Robotic process automation

10- Trizetto

Trizetto is a healthcare company that provides revenue cycle management services to small-scale physician practices, hospitals, and health systems. Their comprehensive RCM support includes coding, billing, AR follow-up, and payment posting. Moreover, their services are compatible with various practice management systems, which makes the billing process convenient and accurate.
This best revenue cycle management company has an AAPC- and AHIMA-certified team of coding professionals who ensure clean claim submissions. In case the claims are denied, Trizetto also provides claims management services, such as claim editing, resubmission, and claim follow-up to help maximize reimbursements.
Its Key Offerings Include
- Tools for eligibility verification and prior authorization
- Claim and payment audits
- Contract management
- Analytics and reporting
Key Factors to Consider When Choosing from Top Revenue Cycle Management Companies
Selecting the best RCM company for your practice is crucial to maximize revenue. Before you partner with one of the top revenue cycle management vendors, here are a few things to consider.
1. Experience and Specialization
The first thing you must consider is the company’s years of experience and level of expertise. A company that has spent more years in the healthcare industry is more likely to have encountered and managed billing-related issues. Additionally, it’s important that the RCM provider has expertise in your medical specialty, as every specialty has unique billing codes and compliance requirements.
2. Scope of Services
Select a revenue cycle management firm that provides end-to-end revenue cycle management services. A top RCM company handles the entire billing process, including insurance eligibility checks, claim submission, denial management, patient collection, and financial reporting. Since the RCM process includes so many complex stages, partnering with a provider that provides all the mentioned services reduces errors and shortens the revenue cycle.
3. Compliance & Certifications
Healthcare organizations must comply with strict regulations like HIPAA to protect patient data. Apart from that, certifications such as HITRUST or SOC 2 provide additional assurance that the provider takes data protection seriously. So, pick a company that invests in advanced security protocols.
4. Technology and Integration
Consider working with a revenue cycle management company that utilizes advanced technologies, such as Artificial Intelligence or Robotic Process Automation, to streamline revenue cycle processes. And for seamless data transfer, check if their systems integrate well with your existing EHR software.
5. Transparency and Reporting
Another important factor that you must look for in an RCM company is the advanced analytics and reporting features. The RCM company you partner with must offer real-time dashboards and detailed reports that track key performance indicators. These insights help you monitor the financial health of your practice and quickly identify issues related to revenue leakage.
6. Pricing Model
Lastly, you should carefully evaluate the pricing model of the RCM company. Some companies charge a certain percentage on the collections, while others may offer a flat fee or a hybrid pricing structure. Pick a company whose pricing structure aligns with your budget and expected ROI.

Conclusion
To conclude, healthcare organizations need to partner with the best revenue cycle management companies to achieve maximum revenue optimization and decrease administrative loads. This guide has provided a list of the top 10 healthcare RCM companies and highlighted the key factors to consider to help you make an optimal choice. Each RCM provider in this list provides expert, end-to-end RCM services that help healthcare organizations bill with greater efficiency and reduce claim denials.
However, among all the RCM companies, Transcure stands out with a 98% first pass clean claim and the ability to boost revenue by up to 10%. So, if you want to eliminate billing errors and maximize your practice’s financial health, choosing a partner like Transcure is the way forward.
Frequently Asked Questions (FAQs)
What is revenue cycle management in healthcare?
Healthcare revenue cycle management refers to the administrative and clinical processes that help providers receive payment for medical services from insurance companies. It involves tasks such as patient registration, eligibility verification, medical coding, claims submission, and payment collection.
Which is the most important stage of the RCM cycle?
Claim processing is a critical stage in RCM that involves accurate coding, timely submission, and minimizing denials. Errors in claims can lead to decreased revenue and delayed payments. Therefore, efficient claims processing is essential for maintaining strong financial operations and steady cash flow in healthcare facilities.
What are the benefits of using an outsourced RCM company versus in-house billing?
Outsourcing RCM offers expert handling of billing, reduces administrative costs, speeds up claim processing, and minimizes errors. Moreover, it provides access to advanced technology and scalability without hiring extra staff. This leads to faster reimbursements, improved cash flow, and allows healthcare providers to focus more on patient care rather than on administrative tasks.
Which is the best revenue cycle management company in the U.S.?
Several companies consistently rank high in terms of market share, client satisfaction, and service offerings. The top RCM companies that are experts in providing RCM services are Transcure, Athenahealth, R1 RCM, eClinicalWorks, and others. However, determining the revenue cycle management company depends on the specific needs of the healthcare provider.









