The Merit-based Incentive Payment System (MIPS) is a Medicare program created by MACRA (2015) and effective in 2017 that merges legacy quality programs. It combines PQRS, Value-Based Modifier, and Meaningful Use into a single pay-for-performance system. Under MIPS, eligible Medicare Part B clinicians receive an annual Composite Performance Score (CPS) from 0 to 100.
Each clinician’s final MIPS score drives their Medicare Part B payment adjustment (up to ±9% in 2025). In practice, high MIPS scores earn bonus payments, while low scores trigger penalties. It is vital for U.S. practices to understand MIPS eligibility and reporting to protect revenue and seize incentive opportunities.
Read this guide to learn everything about MIPS reporting and scoring, and how it can impact your practice’s bottom line.
Table of Contents
ToggleWhat is a Merit-Based Incentive Payment System?
The Merit-based Incentive Payment System (MIPS) is the main part of Medicare’s Quality Payment Program (QPP) that adjusts Part B physician payments based on performance. Established by MACRA and implemented in 2017, MIPS consolidated three earlier programs into one points-based system.
Each year, CMS evaluates participating clinicians across four categories, including Quality, Cost, Improvement Activities, and Promoting Interoperability. Scores in these categories (weighted as 30%, 30%, 15%, and 25% respectively in 2025) are combined into a Composite Performance Score (CPS) on a 100-point scale.
This CPS determines the practice’s Medicare payment adjustment in the following year. So, clinicians with high scores receive bonus payments (up to +9%), and those with low scores incur penalties (up to –9%).
What is MIPS Reporting?
MIPS reporting is the process by which eligible clinicians submit performance data to CMS under the MIPS program. Reporting involves selecting specified measures and activities in the Quality, Improvement, and Promoting Interoperability categories and submitting the required data (via EHR systems, registries, or claims) by CMS deadlines.
For Quality, practices typically report at least six measures (including an outcome measure) covering patient care and outcomes. And for Improvement Activities, they attest to performing selected practice-improvement tasks.
Regarding Promoting Interoperability, they report on the use of certified EHR technology (such as e-prescribing and patient portals). The Cost category is automatically calculated by CMS from Medicare claims.
All submitted data are scored according to national benchmarks, producing performance scores in each category. The MIPS Composite Performance Score (0 – 100) is then computed from the weighted category scores. In essence, MIPS reporting quantifies how well clinicians deliver quality, efficient care – and links that performance to their future Medicare reimbursements.
What are the Goals and Purposes of MIPS Reporting?
MIPS was designed to align Medicare payments with high-value care. The key goals include:
- Improve Quality of Care (Value-Based Care): MIPS reporting services incentivize clinicians to focus on patient outcomes and clinical processes that drive better health.
- Control Healthcare Costs: Such a MIPS consultation encourages efficient use of resources by linking payment to cost measures, rewarding cost-effective care without sacrificing quality.
- Promote Health IT and Interoperability: With MIPS reporting, practices can perform advanced adoption of electronic health record technology to improve care coordination and patient engagement.
- Encourage Practice Innovation: MIPS consulting services motivate providers to implement new care-management and engagement activities through the Improvement Activities category.
- Increase Accountability: MIPS reporting provides transparent feedback on clinician performance and makes Medicare payments contingent on meeting national benchmarks.
How MIPS Evolved Over Time?
Before 2017, Medicare used multiple overlapping quality programs (PQRS for quality measures, the Value Modifier for cost, and Meaningful Use for EHRs). The Medicare Access and CHIP Reauthorization Act (MACRA) of 2015 repealed the Sustainable Growth Rate and created the QPP with two tracks: MIPS and Advanced APMs.
MIPS replaced and consolidated those legacy programs into one unified system. Over the years, MIPS rules have evolved:
- Thresholds and category weights have been updated.
- Reporting options expanded (e.g., virtual groups, MVPs, the APM Performance Pathway)
- Performance benchmarks refined
For instance, in 2023, CMS introduced MIPS Value Pathways (MVPs) as an alternative reporting framework. Despite these changes, MIPS has remained budget-neutral and continues to evolve with annual rulemaking.
Now, CMS is considering making MVPs mandatory by 2028 and adding new MVPs and measures in future years. Through these changes, MIPS has steadily shifted Medicare toward rewarding value and quality while providing clinicians with new reporting flexibility.
What Are the MIPS Eligibility Requirements?
A clinician or group is eligible for MIPS reporting if they meet all three of CMS’s low-volume threshold criteria during the determination period:
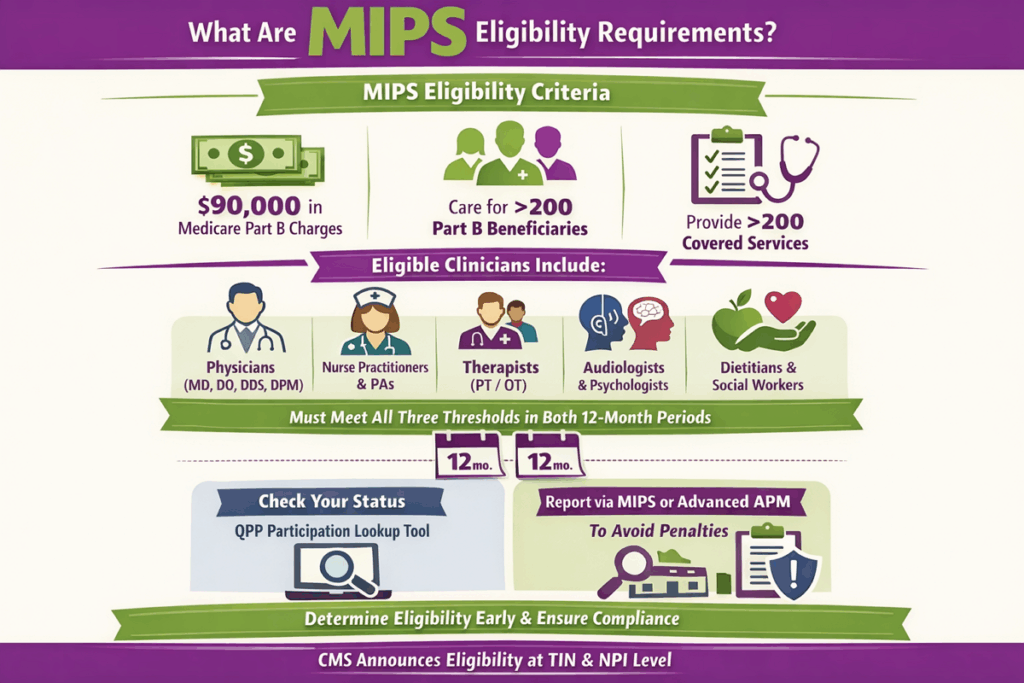
(1) bill >$90,000 for Medicare Part B covered services,
(2) provide care to >200 Part B beneficiaries, and
(3) deliver >200 covered services.
Eligible clinician types include physicians (MD/DO, DDS, DPM), physician assistants, nurse practitioners, clinical nurse specialists, CRNAs, therapists (PT/OT), audiologists, psychologists, dietitians/nutritionists, social workers, and others.
If a clinician or TIN meets all three thresholds for both 12-month segments in the determination period, they are required to participate in MIPS. The eligibility is determined at the Taxpayer Identification Number (TIN) and NPI level and is announced by CMS.
It’s important to verify eligibility early to ensure compliance and planning. CMS provides the QPP Participation Lookup Tool to check if you exceed the thresholds. Practices that qualify must then report via MIPS (or an Advanced APM) to avoid penalties.
Who Has to Report MIPS?
Eligible clinicians who bill Medicare Part B must report MIPS data if they exceed the low-volume thresholds. This includes most physicians and other Part B providers (MD/DO, dentists, optometrists, chiropractors, PAs, NPs, CNS, CRNAs, PT, SLPs, audiologists, psychologists, dietitians, social workers).
Groups that consist of these providers can also report at the group (TIN) level. CMS’s 2025 rules reiterate that clinicians are required to participate if they belong to a MIPS-eligible clinician type and exceed all three threshold elements.
How Do I Know If I Need to Participate in MIPS?
To determine participation:
- Check Eligibility Status: Use CMS’s QPP Participation Status Tool to see if you exceed thresholds.
- Review Billing and Patient Counts: Make sure you bill over $90K and see above 200 Medicare Part B patients/services.
- Consider New Enrollment: If you’re newly enrolled in Medicare, you are exempt from MIPS for that year.
- APM Participation: If you participate in an Advanced APM and attain Qualifying APM Participant (QP) status, you are excluded from MIPS.
Which Practitioners are Exempt from MIPS Reporting?
Some clinicians are excluded from MIPS regardless of their performance:
- New Medicare Enrollees: Providers in their first year of Medicare enrollment are exempt for that performance year.
- Low-Volume Providers: Those who fail to exceed the low-volume thresholds in either determination period segment (bill less than $90K, less than 200 patients) are not required to report.
- Advanced APM Qualifiers: Clinicians who are qualifying APM participants (meaning they earn enough through Advanced APMs) are excluded from MIPS.
What Are the Participation Options for MIPS Reporting?
Practices have multiple ways to participate in MIPS each year.
1. Individual and Group Reporting
Clinicians can report as individuals under their NPI or as part of a TIN group. Groups can be single-specialty or multispecialty. Reporting as a group means one composite score for the entire practice, while individuals report their own data.
2. Virtual Group Reporting
Small practices can form virtual groups (two or more solo practitioners/small groups) to report together. This allows solo providers to combine resources for reporting and be evaluated as a group.
3. MIPS Reporting Paths
There are three main reporting paths:
- Traditional MIPS: The original pathway, where clinicians pick measures from any category (Quality, IA, PI) and submit data as described in CMS guidelines.
- MIPS Value Pathways (MVPs): Launched in 2023, MVPs are specialty/condition-specific bundles of measures and activities. Each MVP includes selected quality measures, one improvement activity, cost measures, and foundational population health and PI measures. MVPs are voluntary through 2027.
- APM Performance Pathway (APP): For providers in a MIPS APM entity, the APP offers a simplified, defined set of measures (often registry-based) to reduce reporting burden.
4. Opt-In/Voluntary Reporting
Clinicians who exceed at least one (but not all) low-volume thresholds can opt in to MIPS voluntarily. Even if not strictly required, opting in allows them to earn positive adjustments.
5. Subgroup Participation
Starting in 2023-25, CMS permits subgroups within larger practices to report MVPs. A subgroup is a subset of a TIN (usually by specialty). Multispecialty groups must form subgroups to use MVPs beginning in 2026.
What are the MIPS Performance Categories?
CMS evaluates performance in four categories, each with specific requirements. The categories are Quality (30%), Cost (30%), Improvement Activities (15%), and Promoting Interoperability (25%). Your scores in these categories are weighted and summed to determine your final MIPS score. Below are the details of each category:
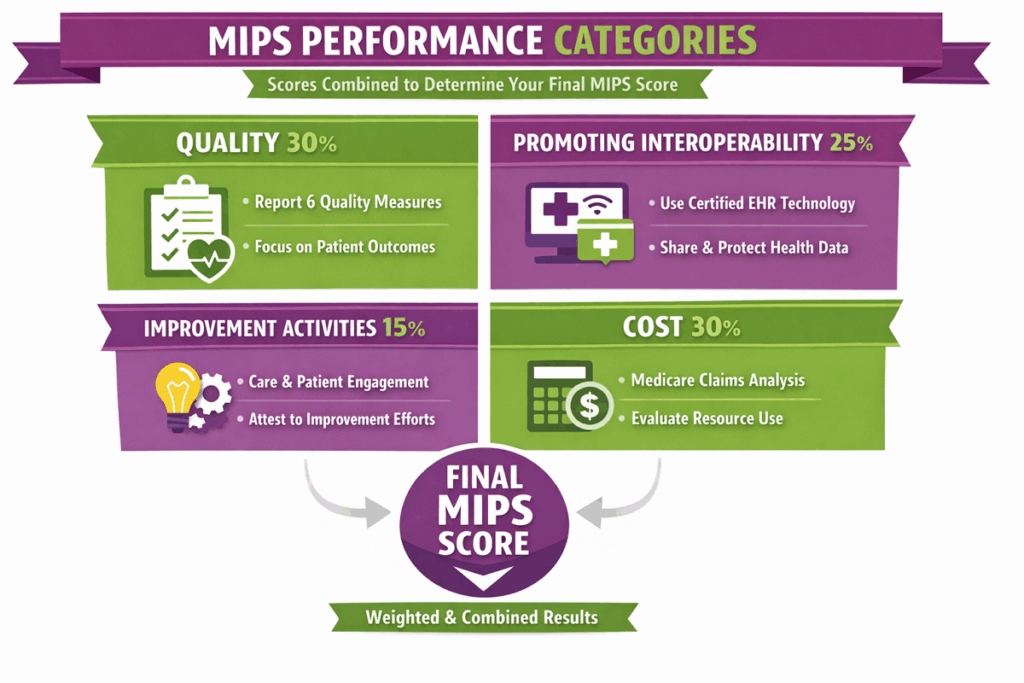
Quality (30%)
This category measures patient care quality and outcomes. Clinicians typically select six quality measures (or a specialty measure set) that best reflect their practice. At least one must be an outcome or high-priority measure.
For each measure submitted, you must report data on at least 75% of eligible patients (75% data completeness) and have a case minimum of 20 patients to receive full points. Performance on these measures is compared to national benchmarks.
(If a measure has no benchmark, it yields minimal points.) Your Quality category score is the sum of achievement points earned across all measures, scaled to 30 points.
Promoting Interoperability (25%)
This MIPS reporting category (formerly Meaningful Use) incentivizes use of certified Electronic Health Record Technology (CEHRT). Clinicians must report on a set of required objectives over a 90- or 180-day period, depending on the measure.
The PI measures assess how well a practice uses EHRs to share information, engage patients, and secure data. Successful reporting yields up to 25 points. (Small practices automatically get PI reweighted.)
Improvement Activities (15%)
With this MIPS consulting category, CMS rewards practices for engaging in care-improvement and patient-engagement activities. CMS publishes a list of approved Improvement Activities (care coordination protocols, patient navigation, telehealth implementation).
To earn full IA credit, clinicians must attest to performing either two medium-weighted activities or one high-weighted activity for at least 90 continuous days in the year. Completing the required IA measures yields up to 15 points.
Cost (30%)
The Cost category in MIPS reporting evaluates the resource use associated with care. Clinicians do not submit data, as CMS calculates the cost score from Medicare claims. CMS measures things like episode-based costs and total per capita costs.
For each relevant cost measure with enough cases, CMS assigns a score and averages them to form your Cost category score. The result is scaled to 30 points. If no cost measures qualify, the cost category is scored as zero or reweighted.
What Determines My Final MIPS Score?
A clinician’s Final MIPS Score (Composite Performance Score) is a weighted sum of the four category scores plus any bonus points.
Final MIPS Score = (Quality Score × 30%) + (Promoting Interoperability Score × 25%) + (Improvement Activities Score × 15%) + (Cost Score × 30%) + Complex Patient Bonus + Small Practice Bonus
Each category score is a percentage of its category weight (scoring 80% on Quality yields 0.8 × 30=24 points).
- CMS may add a bonus (0 to 5 points) for treating a high proportion of complex patients (calculated post-hoc).
- Small practices (≤15 clinicians) automatically receive up to +6 bonus points in the Quality category if they report measures.
The final score (0–100) is then compared against the annual performance threshold to determine payment adjustments. A higher score means a larger positive adjustment, and a lower score yields a negative adjustment.
CMS also includes any Improvement Score (extra points for year-to-year progress) and bonuses when calculating your final score.
MIPS Scoring Example and Benchmarks
CMS publishes benchmarks for each quality measure based on historical performance. If your performance rate on a measure meets the 90th percentile benchmark, you earn the maximum points for that measure. Achieving 0 points (failing to report or meet minimum thresholds) drags down the category score.
Example: Suppose a clinician reports 6 quality measures with a denominator of 100 each, and their performance earns 32 out of 60 total possible quality points. That is 53% of the 60-point potential, which on a 30% weight becomes ~16 points. Add points from the other categories and any bonuses to get the final score.
What are MIPS Value Pathways (MVPs)?
MIPS Value Pathways (MVPs) are an alternative MIPS reporting framework introduced in 2023. Each MVP is a specialty- or condition-specific bundle of measures across the Quality, Improvement Activities, Cost, and Promoting Interoperability categories.
For example, an MVP might include four quality measures (at least one outcome), one improvement activity, and cost measures related to that field, along with a “foundational layer” of population health and required PI measures.
In 2025, CMS finalized 21 MVPs covering areas like Primary Care, Cancer, Heart Disease, Women’s Health, Mental Health, and more. MVPs are voluntary through at least 2027 (traditional MIPS remains available).
How Can You Differentiate Between MVP vs. Traditional MIPS Reporting?
To differentiate MVP and Traditional MIPS reporting, go through this table:
| Feature | Traditional MIPS | MIPS Value Pathways (MVPs) |
|---|---|---|
| Pathway Introduction | Established 2017 under QPP. Original MIPS reporting. | Introduced 2023 (pilot) as a voluntary reporting option. CMS may require it by 2028. |
| Focus | MIPS reporting across all categories. Clinicians pick any measures. | Specialty/condition-focused. Aligns measures across categories relevant to a specific practice. |
| Quality Measures | Select 6 measures (including an outcome or high-priority) for a full year. Benchmarks applied to each measure. | Select 4 measures within the MVP (including one outcome) for a full year. Also includes one CMS-scored population health measure by claims. |
| Improvement Activities | Choose 2 activities (90-day each). | Choose 1 activity (90-day) from the MVP list. |
| Promoting Interoperability | Report the full set of PI measures for 180 days (if applicable). | Same PI measure set for 180 days (unless exempt). |
| Cost Measures | CMS uses all applicable cost measures (claim data) to calculate Cost score. | CMS scores based on cost measures specific to the MVP’s specialty (claims data). |
| Participation Options | Eligible as Individual, Group, or Virtual Group. No subgroups. | Eligible as Individual, Group, or Subgroup (new). Multispecialty groups can form subgroups by specialty for MVP reporting. |
| Reporting Tool | Submit via QPP portal/registry/EHR as usual. | Submit via QPP portal, selecting the chosen MVP and measures. Requires MVP registration each year. |
What are the Specialty-Focused MVP Reporting Options?
CMS has created MVPs for many specialties and conditions. Each MVP is named for its focus and includes relevant measures. Examples include:
- Value in Primary Care: Broad primary care metrics (preventive care, chronic disease management) for general practitioners.
- Advancing Cancer Care: Oncology-focused measures, such as patient experience, end-of-life care, appropriate diagnostics, and treatment for cancer.
- Advancing Care for Heart Disease: Cardiovascular measures such as heart failure therapy, preventive screenings, and more.
- Dermatological Care: Quality measures for skin disease management (melanoma screening, dermatitis control).
- Improving Care for Joint Repair: Orthopedic measures around joint replacement outcomes and rehabilitation (Lower Extremity Joint Repair MVP).
- Quality Care in Mental Health and Substance Use: Behavioral health measures targeting mental health and SUD services.
- Pulmonology Care: Respiratory disease management (asthma/COPD care measures).
- Women’s Health: Measures related to women’s health services (screening, prenatal care).
For 2025, CMS finalized 21 MVPs covering a wide range of specialties. However, for the 2026 performance year, MVPs are expanding with six new specialty-specific pathways for Diagnostic Radiology, Interventional Radiology, Neuropsychology, Pathology, Podiatry, and Vascular Surgery, joining existing MVPs.
How Does MIPS Scoring Impact Your Medicare Reimbursements?
MIPS scoring directly affects Medicare Part B payments. The final MIPS score determines the payment adjustment applied to every Part B claim in the next payment year. In practice:
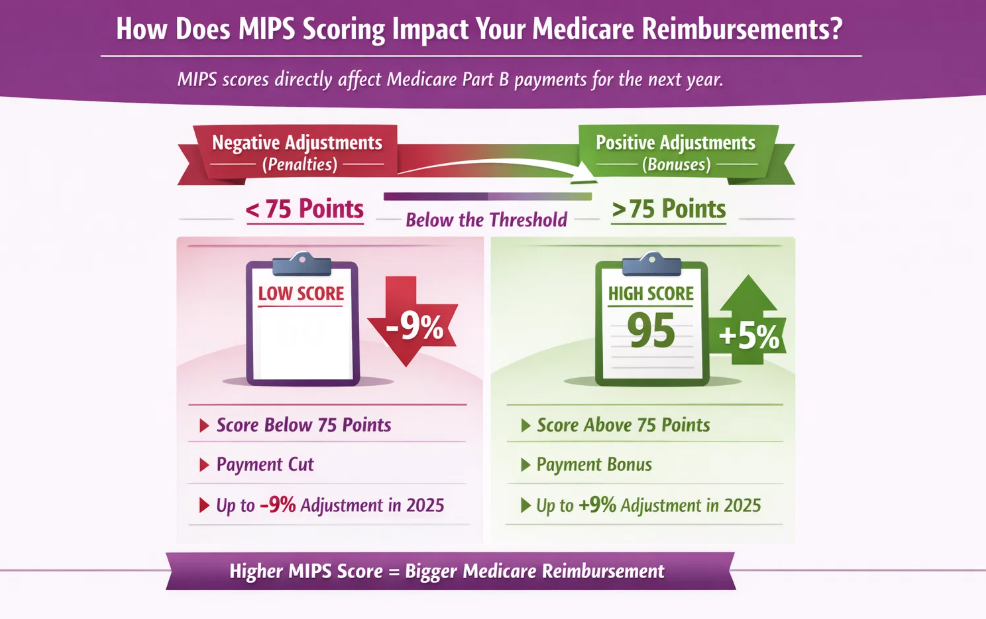
Negative Adjustments (Penalties)
Clinicians who score below the annual performance threshold incur payment cuts. For 2025 reporting, the threshold is 75 points. For example, a final score of 60 in 2025 (below 75) would result in a downward adjustment. CMS adjusts payments on a sliding scale up to the maximum negative adjustment (–9% in 2025).
Positive Adjustments (Bonuses)
Scores above the threshold earn positive adjustments. A final score above 75 will increase Medicare reimbursements. The higher the score (up to 100), the larger the bonus, up to +9% in 2025. For example, a score of 95 might yield a +5% payment bonus (exact rates are budget-neutral and set each year).
Budget Neutrality
MIPS is budget-neutral, so this means bonuses are funded by penalties. High-performing providers get larger increases, while underperforming providers fund those bonuses through their cuts.
Because of this mechanism, MIPS performance has a direct revenue impact. Improving your score by just a few points can translate into thousands of dollars over the year.
What is the Impact of MIPS on Medicare Payments?
Practices with high MIPS scores will receive upward payment adjustments. For example, a small practice that achieves a final score of 95 might earn a several percent bonus on all Medicare Part B payments in the following year.
CMS data show that a significant share of providers receive penalties when thresholds rise. Thus, MIPS performance directly translates to higher or lower Medicare reimbursements. This makes MIPS reporting essential, as good scores protect revenue while poor scores erode it.
What are the Performance Thresholds and Penalties for MIPS?
Each year, CMS sets a performance threshold. For 2025 reporting, that threshold is 75 points. Clinicians must score at least this to avoid penalties. The payment adjustments are then determined on a scale:
- 0 to 75 points: Negative adjustments (more negative the lower the score). In 2025, scores up to 18.75 yield the full –9% penalty, then it scales to 0% at 75.
- 75.01 to 100 points: Positive adjustments. Any score above 75 earns a bonus (the higher the score, the larger the bonus).
What Happens If You Don’t Participate in MIPS Reporting?
Eligible clinicians who fail to report MIPS data face the harshest outcome. Specifically:
- Zero Score: CMS assigns a score of 0 to any eligible clinician who does not submit the required data by the deadline.
- Maximum Penalty: A final score of 0 triggers the maximum downward adjustment. In 2025, that means a –9% payment cut on all Medicare Part B services in the following year.
- No Bonus Opportunity: Non-reporters cannot earn any positive adjustment, so they automatically lose revenue each year.
- Audit Risk: Repeated non-participation could invite CMS inquiries or flags, as eligible clinicians are expected to participate or officially qualify for exclusion.
In short, don’t participate ⇒ 0 CPS ⇒ max penalty. It’s crucial that eligible providers either submit data or formally opt out if legitimately exempt. Most practices simply cannot afford the guaranteed –9% hit, making full MIPS participation (or approved exemption) essential.
How Transcure Helps Practices Get Started with the MIPS Reporting Process?
Transcure offers end-to-end MIPS consulting services to guide practices through every reporting step. Their approach includes:
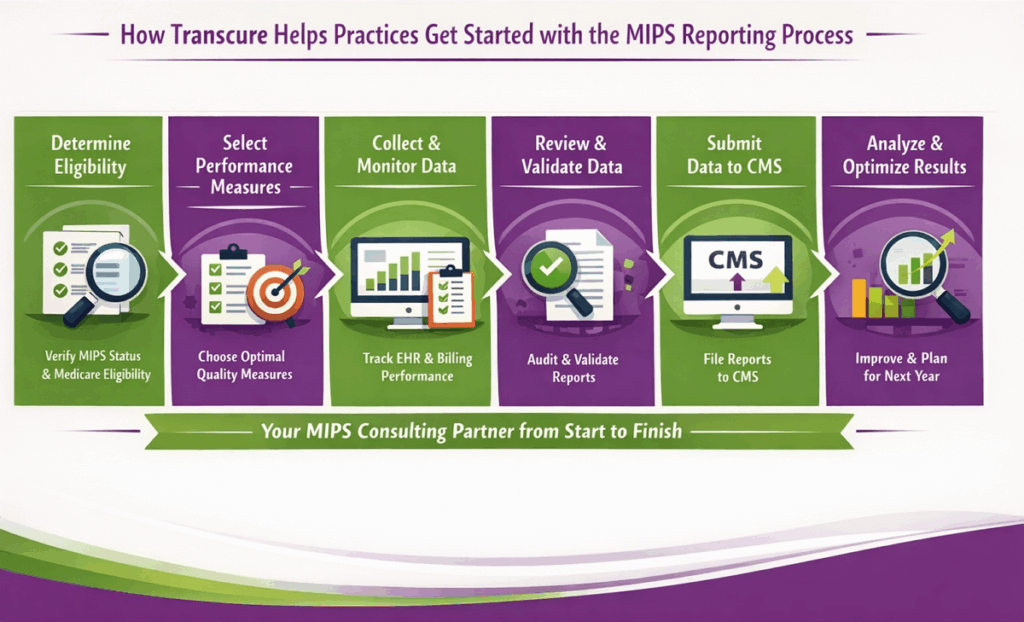
Step 1: Determine Eligibility
Transcure first verifies your MIPS status using CMS criteria and the QPP participation lookup tool. They check your Medicare Part B volumes and beneficiaries to confirm if you must report.
Step 2: Select Performance Measures
Their consultants identify the highest-scoring, most relevant quality measures for your specialty. This strategic selection maximizes your scoring potential (and thus incentive) within Quality and MVPs.
Step 3: Collect and Monitor Data
Throughout the year, Transcure tracks performance data from your EHR and billing systems. Ongoing monitoring allows them to spot gaps and advise adjustments before submission deadlines.
Step 4: Review and Validate Data
Before filing, Transcure’s MIPS experts meticulously audit your data. This minimizes errors or omissions that could otherwise lead to score reductions or CMS audits.
Step 5: Submit Data to CMS
Acting as your MIPS partner, Transcure handles the actual submission via approved portals. They ensure timely, compliant uploads of all measures and attestation data.
Step 6: Analyze Results & Optimize
After CMS assigns your score, Transcure analyzes the feedback. They identify weak areas and recommend improvement strategies for the next year, helping you earn even higher scores in future cycles.

Conclusion
In summary, MIPS is Medicare’s system for shifting payments toward value-based care. It scores clinicians on quality, cost, interoperability, and improvement activities, then adjusts Medicare Part B fees based on those scores. Eligibility depends on Medicare Part B billing thresholds and clinician type.
Overall, high performance yields bonuses (up to +9% in 2025), while failing to report results in significant penalties. Understanding MIPS rules and accurately reporting can protect and even increase a practice’s Medicare revenue.
With complex requirements and evolving rules, many U.S. providers enlist specialized MIPS reporting services. As shown, Transcure offers a guided MIPS solution, so you can focus on patient care.