Neurology practices in the U.S. perform complex and high-volume procedures, including EEGs, EMGs, and nerve conduction studies. Accurate coding for these procedures is critical for timely claim submission. According to the Centers for Medicare & Medicaid Services (CMS), 25% neurology claims are paid incorrectly due to documentation, coding, or wrong modifiers.
Inaccuracies in neurology billing have a significant financial impact on providers. According to PMC, documentation and coding errors in neurology practices can cause annual revenue losses of $33,000 to $100,000 per medium-sized facility.
With growing patient volumes and strict payer requirements, neurology billing requires attention at every step. This is why many providers are turning to specialized neurology billing services to streamline payments and reduce costly errors.
This guide explains the neurology billing process step by step, outlines common billing challenges, and provides updated CPT and ICD-10-CM code cheat sheets for 2026. We will also share practical tips and provide extensive code cheat sheets to help your practice minimize write‑offs.
Table of Contents
ToggleWhat Are the Most Common Neurology Billing Challenges
Neurology practices operate in a high-risk billing environment, with complex diagnostics, strict payer policies, and documentation-intensive services. This creates unique medical billing challenges not commonly seen in other specialties.
1. High Denial Rates For EEG, EMG, And NCS Procedures
Neurology claims for diagnostic testing are frequently denied due to missing documentation, incorrect code selection, or failure to meet payer-specific medical necessity criteria. EEGs, EMGs, and nerve conduction studies often require detailed clinical notes, test interpretations, and accurate CPT code sequencing.
2. Authorization Delays And Payer Restrictions
Many neurology procedures, such as Lumbar Puncture (CPT 62270, 62272) and Deep Brain Stimulation (DBS) implantation (CPT 61863), require prior authorization. Delays or missing authorizations can result in claim denials or extended reimbursement timelines, affecting cash flow.
3. Modifier Misuse And Incorrect Application
Neurology billing relies heavily on modifiers such as 25, 26, TC, and 59. Incorrect or inconsistent modifier usage can result in bundling issues, partial payments, or claim rejections.
4. Underpayment And Bundling Challenges
Payers might bundle neurology procedures incorrectly or reimburse only the technical or professional ones. This leads to underpayments when claims are not carefully reviewed and appealed.
5. Complex Documentation For Multi-Visit Neurology Care
Neurology often involves ongoing, multi-visit management of chronic conditions. Capturing all relevant symptoms, assessments, and treatment decisions for accurate coding is difficult, and omissions can lead to claim denials or audits.

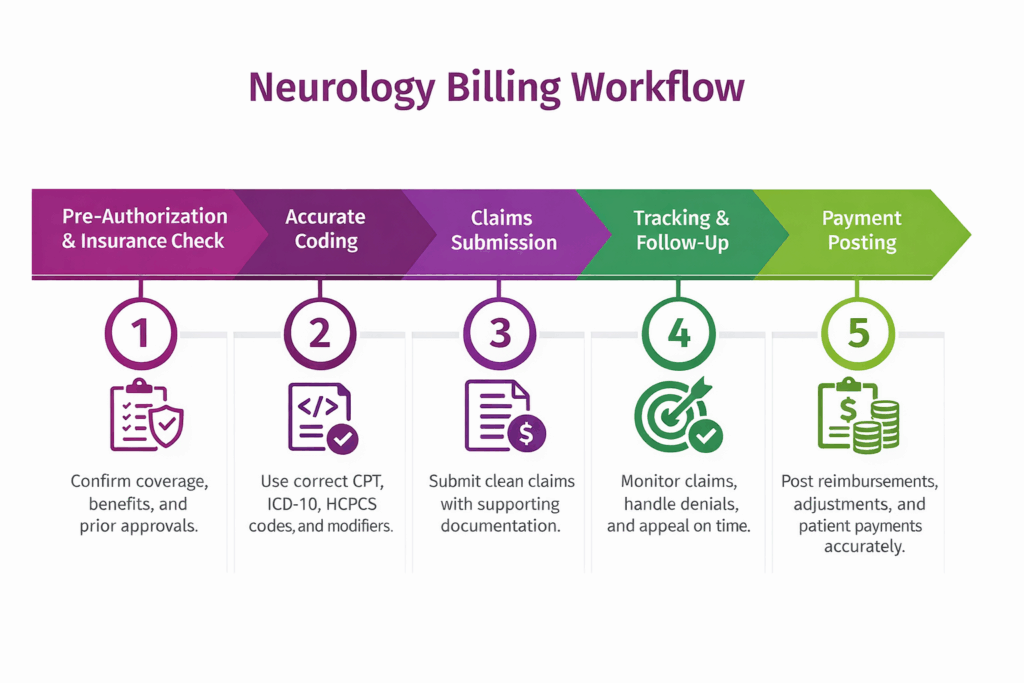
A Comprehensive Neurology Billing and Coding Workflow
Neurology billing requires precise coding and proper documentation. High-volume procedures, chronic patient management, and payer-specific requirements make accurate billing essential to avoid revenue loss. We have enlisted the steps in the neurology medical billing process to help your practice maximize reimbursements.
Step 1: Pre-Authorization and Insurance Eligibility Verification
Pre-authorization and insurance eligibility verification are critical processes in neurology billing. Neurology services are high-cost and tightly regulated by payers, requiring strict compliance. Before scheduling or providing services, practices must verify active insurance coverage, plan benefits, deductibles, and coverage limits for procedures such as nerve blocks, spinal cord stimulator implants, or lumbar injections.
Prior authorization is often required for advanced diagnostics and interventional neurology procedures, such as CT Angiography. In addition, referral requirements and in-network provider status must be confirmed, especially for HMO and managed care plans.
Step 2: Accurate Coding and Capturing Charges
Accurate charge capture is crucial in neurology billing, as even minor coding errors can lead to denials, underpayments, or compliance risks. Neurology billing services must be coded using the correct codes for procedures and evaluations.
- CPT Codes: Used to describe medical procedures and services performed by the neurologist. For example, Cervical epidural injection (CPT 62310), Peripheral nerve block (CPT 64450), 95816 (EEG)
- ICD-10-CM Codes: Used to identify the patient’s medical diagnosis for billing and insurance purposes. For example G43.909 (Migraine), G40.909 (Epilepsy)
- HCPCS Codes: Used for supplies, medications, and durable medical equipment not covered by CPT. For example, J3030 (Injection, sumatriptan), E0760 (Cervical traction device)
- Modifiers: Used to provide additional information about a service. For examples -25 (Significant E/M), -59 (Distinct procedural service)
- Prolonged Service Codes: Used to bill for extended time spent with a patient beyond standard E/M visits. For example, 99205 (New patient, prolonged), 99215 (Established patient, prolonged)
Each service provided must be fully documented and supported by clear clinical documentation. Practices must also avoid undercoding, which leads to revenue loss, and overcoding, which increases audit and denial risk.

Step 3: Claims Submission
Creating a clean claim requires accurate CPT and ICD-10-CM coding, correct modifier usage, and alignment with prior authorization details. Most neurology claims are submitted electronically to reduce processing time and minimize manual errors.
Supporting documentation, such as physician notes, test interpretations, and medical necessity justification, is required, especially for neurodiagnostic testing. Common rejection reasons include missing or invalid authorizations, diagnosis-procedure mismatches, bundled service conflicts, and incorrect modifiers.
Step 4: Claims Tracking and Follow-Up
After claims are submitted, tracking and follow-up ensure timely reimbursement in neurology practices. It’s important because high-cost procedures like EEGs, EMGs, and nerve conduction studies are prone to denials. Continuous monitoring helps identify delayed or unpaid claims early. Best methods for claim tracking include:
- Claim monitoring processes: Using dedicated dashboards to track submission status, remittance, and pending claims in real time.
- Denial identification: Quickly flag denied or underpaid claims caused by missing documentation, incorrect modifiers, or prior authorization issues.
- Appeal timelines: Adhere strictly to payer deadlines for appeals to maximize reimbursement chances.
- Follow-up best practices: Maintain detailed logs, communicate with payers, and resubmit corrected claims promptly to reduce revenue loss.
Effective follow-up ensures that denied or delayed claims do not turn into long-term financial leakage for neurology practices.
Step 5: Payment Posting
Payment posting ensures that all insurance reimbursements and patient payments are accurately recorded. Proper posting helps identify discrepancies, underpayments, and adjustments that can affect your practice revenue.
Key elements of payment posting include:
- Era And Eob Posting: Apply electronic remittance advice (ERA) and explanation of benefits (EOB) details to patient accounts, including CPT/ICD-10 allocations.
- Adjustments and Write-Offs: Record contractual adjustments, denials, or uncollectible amounts for accurate revenue
- Secondary Insurance Handling: Coordinate benefits with secondary payers to capture remaining eligible reimbursements.
- Patient Responsibility Posting: Accurately post copays, coinsurance, and deductibles to ensure transparent patient billing.
In neurology practices, accurate payment posting for high-cost procedures prevents revenue leakage and ensures timely financial reconciliation.
Neurology Billing Coding Cheat Sheet 2026
Neurology billing involves complex diagnoses, recurring patient care, and high-cost therapies. Because most neurological conditions are chronic and progressive, practices depend on accurate coding for long-term revenue. As even small errors can cause denials or payment delays, the following is a neurology coding cheat sheet for 2026:
1. ICD-10 Diagnosis Codes
ICD-10 diagnosis codes show the medical necessity for advanced neurological testing, injections, and infusion therapies. Chronic conditions that require continuous management, frequent follow-ups, and expensive medications need accurate coding for payer approval.
| Category | ICD-10 Code | Description |
|---|---|---|
| Multiple Sclerosis | G35 | Disease-modifying therapy, chronic management |
| Parkinson’s Disease | G20 | Long-term medication and therapy management |
| Alzheimer’s Disease | G30.xx | Cognitive assessment, high follow-up volume |
| Chronic Migraine | G43.7 | Frequent Botox injections and treatments |
| Epilepsy, refractory | G40.3x | Complex seizure management, anti-epileptic drugs |
| Neuropathy (diabetic/idiopathic) | G60–G64 | EMG/NCS studies, high repeat testing |
| Stroke, follow-up | I63.xx | Post-stroke rehab and therapy visits |
| Cerebral palsy | G80.x | Neurological assessments, therapy coordination, and spasticity management |
2. CPT Procedure Codes
CPT procedure codes cover diagnostic studies, therapeutic procedures, and patient visits. High-volume services such as EMG, nerve conduction studies, EEGs, Botox injections, and chronic care visits generate high revenue when coded accurately.
Neurodiagnostic Testing
Neurodiagnostic tests analyze the nervous system’s electrical activity and structure to diagnose conditions of the brain, spinal cord, nerves, and muscles, such as epilepsy, nerve damage, and multiple sclerosis.
| CPT Code | Description |
|---|---|
| 95812 | EEG, routine, awake |
| 95816 | EEG, awake and sleep |
| 95860 | Needle EMG, one extremity |
| 95861 | Needle EMG, two extremities |
| 95907 | Nerve conduction studies, 1–2 studies |
| 95911 | Nerve conduction studies, 9–10 studies |
Chemodenervation & Botox Injection Codes
Chemodenervation with Botulinum Toxin (Botox) injections involves injecting neurotoxins into muscles to temporarily block nerve signals.
| CPT Code | Description |
|---|---|
| 64615 | Chemodenervation for chronic migraine |
| 64642 | Chemodenervation, 1 extremity |
| 64643 | Each additional extremity |
| 96372 | Therapeutic injection, subcutaneous or intramuscular |
| 20553 | Injection, multiple trigger points |
Infusion Therapy Administration
Infusion therapy delivers medication directly into the bloodstream (or other body areas) through a needle or catheter.
| CPT Code | Description |
|---|---|
| 96365 | IV infusion, therapeutic, up to 1 hour |
| 96366 | Each additional hour of infusion |
| 96367 | Additional sequential infusion |
| 96368 | Concurrent infusion |
| 96413 | IV infusion for biologic or specialty drugs |
Chronic Care Management & Remote Patient Monitoring
| CPT Code | Service Type | Description | Typical Neurology Use |
|---|---|---|---|
| 99490 | CCM | 20 min/month clinical staff time | MS, Parkinson’s, epilepsy |
| 99439 | CCM (add-on) | Each additional 20 min | Complex chronic patients |
| 99457 | RPM | 20 min/month treatment management | Seizure tracking, migraine logs |
| 99458 | RPM (add-on) | Each additional 20 min | High-touch monitoring |
Evaluation & Management (E/M)
E/M codes capture patient visits for counseling, care coordination, and follow-up. They are commonly billed with neurology treatments.
| CPT Code | Description |
|---|---|
| 99214 | Established patient, moderate complexity |
| 99215 | Established patient, high complexity |
| 99204 | New patient, moderate complexity |
| 99205 | New patient, high complexity |
| 99417 | Prolonged outpatient service (add-on) |
3. Modifier Codes
Modifiers are used to clarify how services were delivered, prevent incorrect bundling, and ensure full reimbursement. Accurate modifier usage is especially important for spasticity injections, nerve conduction studies performed separately, and tele-neurology evaluation visits.
| Modifier | Description | Neurology Use Case |
|---|---|---|
| -25 | Significant, separately identifiable E/M service | E/M visit billed same day as Botox or EMG |
| -26 | Professional component | Physician interpretation of EEG or EMG |
| -TC | Technical component | Equipment and technician portion of the EEG |
| -59 | Distinct procedural service | Separate EMG and NCS on different nerves |
| -51 | Multiple procedures | Multiple nerve blocks in one session |
| -95 | Telehealth service | Tele-neurology office visits |

4. HCPCS Drug & Supply Codes
HCPCS codes are used for injectable medications, infusion drugs, and medical supplies commonly used in neurology practices. These codes are critical for billing therapies such as migraine injections, multiple sclerosis infusions, and neurological medications.
| HCPCS Code | Drug / Supply | Description |
|---|---|---|
| J0585 | OnabotulinumtoxinA | 1 unit, chronic migraine |
| J2323 | Natalizumab | 1 mg infusion, MS therapy |
| J1623 | Fingolimod | 0.5 mg capsule |
| J1740 | Injection, IC treatment | Spasticity or rare neurodegenerative disorders |
| J3490 | Unclassified drugs | Off-label neurology treatments |
| A4216 | Sterile water/saline | Per 10 mL |
| A4221 | Infusion supplies/pump | Each |
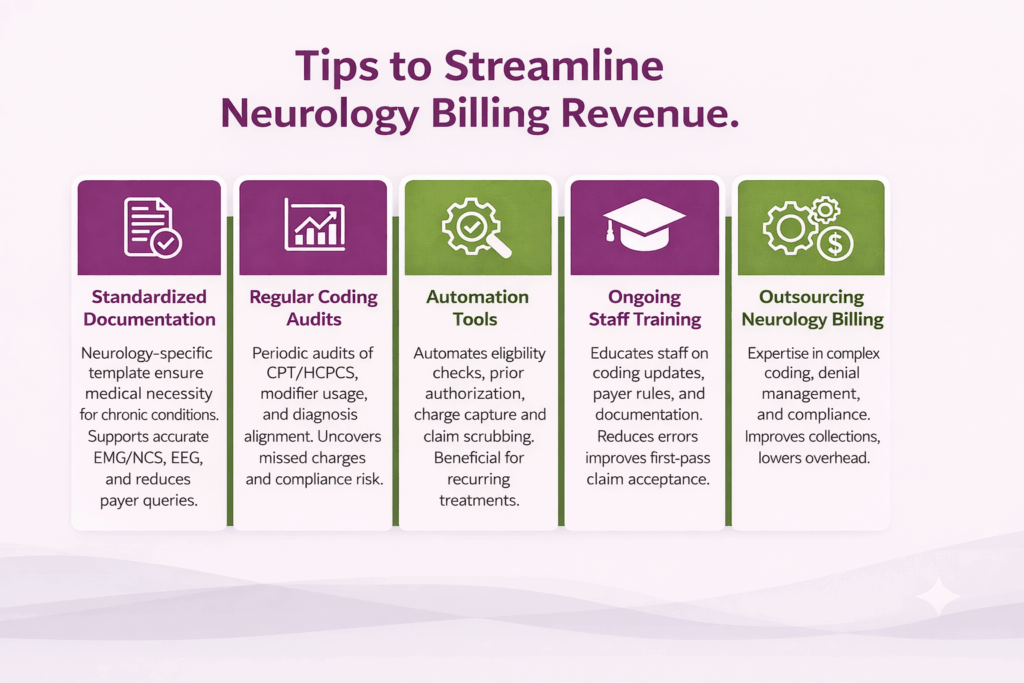
How Can Neurology Practices Streamline Billing and Increase Revenue
Streamlining billing workflows helps reduce denials, accelerate reimbursements, and protect revenue from undercoding or documentation gaps. The following strategies address the most common operational challenges faced by neurology practices.
- Standardized Documentation: Implement neurology-specific documentation templates to capture medical necessity for chronic conditions, diagnostic testing, and time-based procedures. Consistent documentation supports accurate coding for EMG/NCS, EEG, infusion therapies, Botox injections, and high-level E/M services while reducing payer queries.
- Regular Coding Audits: Conduct periodic audits focused on neurology CPT and HCPCS usage, modifier application, and diagnosis-to-procedure alignment. Audits help uncover missed charges, compliance risks, and denial patterns tied to high-ticket neurology services.
- Automation Tools: Use automation for eligibility checks, prior authorization tracking, charge capture, and claim scrubbing. Automation is especially valuable for neurology practices due to recurring treatments and authorization-heavy procedures.
- Ongoing Staff Training: Train billing and clinical staff on neurology-specific coding updates, payer rules, and documentation standards. Continuous education reduces errors and improves first-pass claim acceptance.
- Outsourcing Neurology Billing: Partnering with a neurology-focused billing company such as Transcure provides expertise in complex coding, denial management, and payer compliance. It improves collections, lowers overhead, and allows providers to focus on patient care.

Conclusion
Accurate neurology medical billing is important for maximizing revenue, minimizing denials, and ensuring compliance across complex procedures. By following a structured medical billing process from pre-authorization and precise coding to claims submission and payment posting, neurology practices can streamline operations and improve cash flow. Using CPT and ICD-10-CM codes correctly helps practices reduce errors, improve reimbursements, and focus on delivering high-quality patient care.
Frequently Asked Questions (FAQs)
1. Which CPT codes are commonly used for neurology diagnostic and interventional procedures?
The most common CPT codes for neurology diagnostic and interventional procedures include 95907–95913 for nerve conduction studies, 64615 for chemodenervation for chronic migraine, 64642–64643 for chemodenervation of extremity muscles, 96365–96368 for intravenous infusion therapy, and 99214–99215 for established patient E/M office visits.
2. What CPT codes are used for Botox and chemodenervation in neurology billing?
Chemodenervation in neurology is billed using CPT 64615 for chronic migraine and 64642–64643 for extremity-based injections, along with HCPCS J0585 for onabotulinumtoxinA dosing.
3. Why are neurology claims denied even when correct codes are submitted?
Neurology claims are denied due to missing prior authorizations, insufficient medical necessity documentation, incorrect modifier usage, or payer-specific billing rules, even when CPT and diagnosis codes are accurate.
4. How do modifiers affect reimbursement in neurology billing?
Modifiers such as 25, 26, TC, and 59 clarify service circumstances in neurology billing. Incorrect modifier application can result in bundling issues, partial payments, or claim rejections.
5. What is the CPT code for a neurology appointment?
Neurology appointments use E/M CPT codes such as 99202–99205 for new patients and 99212–99215 for established patients, based on medical decision-making or time.
6. Can teleneurology visits be billed using standard E/M codes?
Yes, most 99204–99215 codes can be used if the visit meets time and complexity requirements, even when delivered virtually.