Chronic kidney disease affects around 35.5 million people in the United States, influencing approximately 14 % of adults. With such high prevalence, the demand for specialized nephrology care is increasing, and so is the need for accurate nephrology billing.
Through nephrology billing services, billers convert kidney care services into standardized CPT, ICD-10, and HCPCS codes. Once the coding is done, bills are submitted to insurance for reimbursement. Even small coding or documentation errors can lead to claim denials, delayed payments, or compliance risks.

To manage this complexity, many providers rely on professional nephrology billing services to ensure efficient revenue cycle management. This guide explains everything you need to know about nephrology billing. You’ll get to learn its billing process, commonly used codes, dialysis and ESRD guidelines, documentation requirements, challenges, and best practices for effective reimbursement.
Table of Contents
ToggleWhat is Nephrology Billing?
Nephrology billing refers to the systematic process of recording, coding, and submitting healthcare claims for services provided to patients dealing with kidney-related conditions. This includes documenting procedures, such as dialysis treatments, kidney function evaluations, laboratory testing, vascular access management, and chronic care services.
The goal is to accurately translate these clinical services into recognized billing codes, such as CPT, HCPCS, and ICD-10. With this process, billers facilitate appropriate reimbursement from private insurers, Medicare, or Medicaid. It supports the financial health of nephrology practices and ensures compliance with federal regulations.
What are the Common Nephrology Services?
Common Nephrology Services include:
- Outpatient and Inpatient Consultations: Evaluation and management of kidney-related conditions.
- Chronic Kidney Disease (CKD) Management: Monitoring, medication management, and disease progression tracking.
- End-Stage Renal Disease (ESRD) Care: Dialysis supervision and monthly physician management.
- Dialysis Services: Hemodialysis, peritoneal dialysis, and home dialysis support.
- Acute Kidney Injury (AKI) Management: Hospital-based evaluation and treatment planning.
- Hypertension and Electrolyte Disorders: Renal-related blood pressure and fluid/electrolyte management.
- Nephrology Procedures: Renal biopsies, dialysis access procedures, and catheter management.
- Laboratory and Diagnostic Review: Kidney function tests, urinalysis, and imaging interpretation.
What is the Overview of the Nephrology Billing Process?

Overall, the nephrology billing process ensures each service is documented, coded, submitted, and paid correctly. Some of its main sub-processes involve the following:
- Pre-Registration and Eligibility: Before services are rendered, nephrology billing often includes verifying patients’ insurance coverage to determine what services are covered and what out-of-pocket expenses the patient may incur.
- Charge Capture and Coding: The billing team records all nephrology-specific services, including dialysis sessions, vascular access procedures, and lab tests, using accurate CPT, ICD-10, and HCPCS codes.
- Claim Submission: Once you have correctly matched CPT and ICD codes, claims for nephrology services are submitted electronically to payers.
- Denial Management: In case you encounter rejection, identify denied claims and take corrective action, such as modifying and resubmitting claims.
- Payment Posting: Upon managing the denials one by one, apply payments from insurers and patients to the accounts.
- Follow-Up: Keep an eye on each submitted claim and pursue overdue payments from payers or patients.

What are the Common Nephrology Coding and Billing Codes?
Nephrology practices must use the correct CPT and ICD‑10 codes for all procedures and diagnoses to ensure accurate and compliant billing. The tables below provide a quick reference to the most commonly used codes in nephrology.
Common CPT Codes in Nephrology Billing
| CPT Code | Description |
|---|---|
| 90935 | Hemodialysis procedure with single physician evaluation |
| 90937 | Hemodialysis procedure requiring repeated evaluations |
| 90940 | Hemodialysis access flow study (vascular access monitoring) |
| 90945 | Dialysis procedure other than hemodialysis (e.g., peritoneal) |
| 90947 | Dialysis other than hemodialysis, with repeated evaluations |
| 90951 | ESRD monthly capitation payment (adult, routine dialysis) |
| 90952 | ESRD monthly capitation payment (alternate visit structure) |
| 90960 | ESRD care, four or more visits during the month |
| 90961 | ESRD care, two to three visits during the month |
| 90962 | ESRD care, one visit per month |
| 90966 | Home hemodialysis services for adults (ESRD) |
| 90967 | Dialysis care management for infants under two |
| 90968 | Dialysis management for children aged 2–11 |
| 90969 | Dialysis management for teens aged 12–19 |
| 90970 | Dialysis management for adults aged 20 and over |
| 90989 | Dialysis training, complete program |
| 90993 | Partial dialysis training session |
| 36147 | Dialysis circuit evaluation, including imaging/blood flow |
| 36558 | Tunneled dialysis catheter insertion |
| 99211 – 99215 | Established outpatient E/M visits (CKD follow-up) |
| 99221 – 99223 | Initial inpatient visits (kidney care) |
| 99490 | Chronic care management (CCM) services |
| 50200 | Renal biopsy, percutaneous |
| 50360 | Renal transplant surgery |
Common ICD-10 Codes in Nephrology Billing
| ICD‑10 Code | Diagnosis / Condition |
|---|---|
| N18.1 | Chronic kidney disease, stage 1 |
| N18.2 | Chronic kidney disease, stage 2 |
| N18.3 | Chronic kidney disease, stage 3 (moderate) |
| N18.4 | Chronic kidney disease, stage 4 (severe) |
| N18.5 | Chronic kidney disease, stage 5 |
| N18.6 | End‑stage renal disease (ESRD) |
| N18.9 | Chronic kidney disease, unspecified |
| N17.9 | Acute kidney failure, unspecified |
| N19 | Unspecified kidney failure |
| I12.9 | Hypertensive chronic kidney disease without heart failure |
| I12.0 | Hypertensive CKD with stage 5 or ESRD |
| Z99.2 | Dependence on renal dialysis |
| Z94.0 | Kidney transplant status |
| T82.4x | Complication of vascular dialysis catheter |
| N25.81 | Secondary hyperparathyroidism of renal origin |
| D63.1 | Anemia in chronic kidney disease |
Common Modifiers in Nephrology Billing
| Modifier | Purpose / Usage |
|---|---|
| 25 | Significant, separately identifiable E/M service on the same day as another procedure, like a nephrology office visit with a procedure. |
| 59 | A distinct procedural service not normally reported together clarifies separate kidney procedures. |
| 26 | Professional component only, used when the provider bills only for the interpretation of a service. |
| TC | Technical component only, indicates facility or equipment costs separate from provider service. |
| 50 | Bilateral procedure, used when a service (e.g., imaging) is performed on both sides. |
| 51 | Multiple procedures performed in the same session by the same provider. |
| 22 | Increased procedural services due to additional work or complexity. |
| 91 | Repeat clinical diagnostic laboratory test on the same date. |
| 76 | Repeat procedure or service by the same provider on the same day. |
| 77 | Repeat procedure by a different provider on the same day. |
| 24 | Unrelated E/M service during a postoperative period. |
| 79 | Unrelated procedure during the postoperative period. |
| 52 | Reduced services, when the service provided is partially reduced or eliminated. |
| 53 | Discontinued procedure due to circumstances like patient request or safety concerns. |
| RT | Right side procedure indicated. |
| LT | Left side procedure indicated. |
| XE | Separate encounter, service is distinct because performed on a separate encounter. |
| XS | Separate structure, service performed on a different anatomical structure. |
| XP | Separate practitioners, distinct services by different practitioners. |
| XU | Unusual non-overlapping service not typically reported together. |

What Are the Essential Dialysis Billing Rules Every Nephrology Practice Must Know?
To ensure timely reimbursement and compliance, nephrology practices must follow the following important dialysis billing rules:
1. Correct Use of Monthly Capitation Payment (MCP) Codes
Medicare reimburses physician management of ESRD patients under Monthly Capitation Payment (MCP) codes rather than per-visit billing. These codes represent all routine outpatient dialysis-related care provided during a calendar month. Only one MCP may be billed per patient per month, regardless of the number of visits.
2. MCP Billing Must Occur After the Month Ends
MCP claims must be submitted only after the calendar month is complete. Billing before the month-end results in automatic claim rejection because Medicare cannot confirm that all required services were delivered during the full billing period.
3. One MCP per Patient per Month Rule
Medicare allows only one MCP payment per ESRD patient per month, even if care is shared or the patient changes dialysis settings. Duplicate MCP claims for the same month will result in denials or recoupments.
4. Face-to-Face Visit Requirements
To bill an MCP, nephrologists must perform at least one documented face-to-face visit with the dialysis patient during the month. Documentation must support a comprehensive monthly assessment, including review of dialysis adequacy, labs, medications, and care planning.
5. Partial Month Dialysis Billing Rules
When dialysis services are provided for less than a full month, such as at treatment initiation, transfer, hospitalization, or death, practices must bill per-diem ESRD management codes instead of a full MCP. Units must reflect the exact number of days managed.
6. ESRD Prospective Payment System (PPS) Bundling Rule
Under Medicare’s ESRD PPS, most dialysis-related services, including labs, supplies, and certain medications, are bundled into a single payment to the dialysis facility. Providers may not bill Medicare separately for services that fall under consolidated billing.
7. Frequency Limits for Dialysis Treatments
Medicare typically covers up to three dialysis sessions per week, calculated as 13 treatments in a 30-day month or 14 in a 31-day month. Claims exceeding frequency limits require strong medical justification, or they will be denied.
8. Hemodialysis vs. Peritoneal Dialysis Billing Differences
In-center hemodialysis and home dialysis, including peritoneal dialysis) follow different billing rules and MCP code sets. Using incorrect codes for the dialysis modality can lead to denials and payer audits.
9. Home Dialysis Management Rules
For home dialysis patients, specific MCP codes must be used. Although fewer in-person encounters may be required, providers must still document monthly clinical management, patient education, and treatment oversight to support billing.
10. Dialysis Training Billing Guidelines
Medicare allows separate reimbursement for home dialysis training sessions, but only within defined limits. Training beyond allowed sessions requires clear documentation of medical necessity, or reimbursement may be denied.
11. Correct Use of Condition Codes
Dialysis claims often require condition codes to identify treatment settings, such as home dialysis, training periods, or transient dialysis. Missing or incorrect condition codes can delay claim processing or trigger rejections.
12. Prohibition on Unbundling Dialysis Services
Billing individual services that are already included in the ESRD bundle, such as routine labs or dialysis supplies, is considered unbundling. This practice can lead to overpayment demands, audits, and compliance penalties.
How to Improve Documentation to Support Nephrology Billing?
To get the most from nephrology coding and billing, it’s important to focus on documentation. As a nephrologist, the notes and records you keep for each patient have a direct impact on your ability to report services accurately.
Be Detailed in Your Notes
When documenting a patient visit, be sure to fully describe the reason for the visit, your exam findings, any diagnoses, and your recommended treatment plan. Notes should specify if services like dialysis were provided, including details about the patient’s condition, any changes since the last visit, and how you are managing chronic conditions.
Use the Proper Codes
Selecting the correct CPT and ICD-10 codes to represent the services provided is key. For example, use specific codes for dialysis, kidney biopsies, and other procedures. Codes for evaluation and management (E/M) visits should match the level of complexity. If counseling or care plan oversight was involved, note the time spent. These details help justify the codes on claims.
Bill for Your Time
Don’t forget to bill for time spent on non-face-to-face services like reviewing records or consulting with other physicians. Codes 99358 and 99359 allow you to bill for prolonged care management. Be sure to document the tasks performed and the total time spent.
Track Quality Measures
Participating in quality reporting programs like MIPS can earn you bonuses, but you need good documentation to support the measures. For nephrology, focus on measures related to anemia management, dialysis adequacy, and transplant waiting. Your notes should clearly indicate how you are meeting recommended guidelines for conditions and procedures.
What are the Major Challenges in Nephrology Billing?
Major challenges in nephrology billing are as follows:
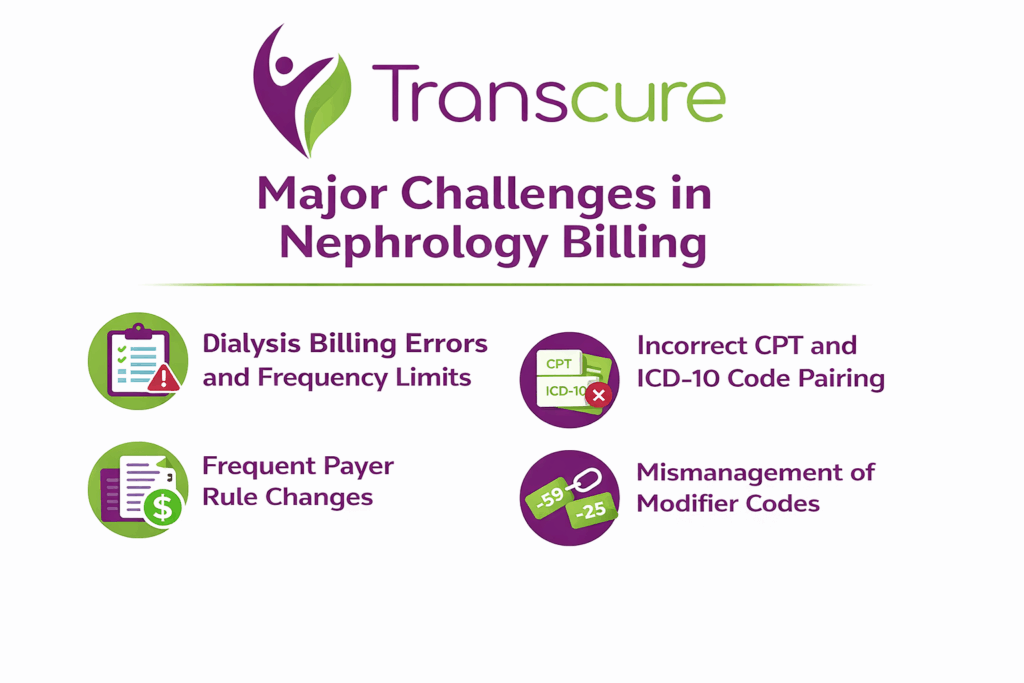
Dialysis Billing Errors and Frequency Limits
Dialysis billing errors are among the most common and costly issues in nephrology due to the complexity of hemodialysis and peritoneal dialysis billing structures. Monthly services are typically billed under Monthly Capitation Payment (MCP) codes, and exceeding frequency limits can trigger automatic denials. Additionally, because dialysis services are often bundled, billing an excluded service separately may result in overpayment demands or audits.
Incorrect CPT and ICD-10 Code Pairing
Another major challenge in nephrology billing is the incorrect pairing of CPT and ICD‑10 codes. Sometimes, the ICD‑10 codes do not support the medical necessity of the billed CPT procedures, chronic kidney disease stage documentation may be incomplete, and comorbid conditions are often underreported. These mismatches can lead to claim denials and increased administrative workload.
Frequent Payer Rule Changes
Frequent payer rule changes pose a significant challenge in nephrology billing, particularly with Medicare’s ESRD Prospective Payment System (PPS) and Medicaid coverage variations. Each payer has unique rules for coverage, bundling, and documentation. Staying compliant with updates, such as CMS manual updates for dialysis services, adds an administrative burden and increases the risk of claim denials.
Mismanagement of Modifier Codes
Modifiers represent service or procedure changes. Modifier misuse, such as using the wrong modifier or missing one, can affect reimbursement and lead to claim rejections, especially for bundled procedures. Inconsistent modifier use across claims might cause misunderstanding and payment issues.

What are the Compliance Considerations for Nephrology Coding and Billing?
There are a few important considerations to keep in mind to stay compliant with laws and regulations in nephrology coding and billing. As a nephrologist, you want to make sure you are properly documenting services, using approved codes, and meeting quality reporting requirements.
Documentation
Proper documentation is key. Clearly record the medical necessity for tests, procedures, and treatments. Note the patient’s symptoms and medical history, your analysis of any test results or scans, the complexity of the case, time spent, and your recommendations. Thorough documentation will support the codes you choose to bill.
Code Correctly
Choose billing codes that accurately reflect the level of service provided. For example, don’t bill a higher level of evaluation and management service than is warranted based on the documentation. Make sure any procedures you perform are billed with the proper CPT nephrology codes. Codes change frequently, so stay up-to-date with the latest code updates.
Meet Quality Reporting Requirements
Participate in programs like the Merit-based Incentive Payment Systems (MIPS) to meet quality reporting requirements. Submit data on quality measures such as lowering high blood pressure, reducing hospital admissions, and improving patient satisfaction. High performance on these measures can qualify you for incentive payments.
Audit Yourself
Conduct regular audits of your own billing and coding practices to catch any errors. Review documentation, codes used, and quality reporting data to ensure you are meeting compliance standards. Make corrections as needed to avoid penalties, claims denials, or audits from insurance payers.
Which is better? In-House vs Outsourced Nephrology Medical Billing
In medical billing, there are two main models practices use to handle claims and revenue cycle management: In-House Billing and Outsourced Billing. Below is a side-by-side look at each so you can decide which model makes the most sense for your nephrology practice.
In-House Billing Model
In-house billing means your practice hires and manages billing staff internally. This team handles eligibility verification, coding, claims submission, denials follow-up, payment posting, and A/R management directly within your office. Practices keep full control of billing operations but also absorb all associated costs.
Price (Typical Costs)
In-house billing requires salaries, benefits, training, and technology. Annual billing staff salaries alone can easily be $140,000–$200,000+, with additional expenses for software, EHR integration, and compliance tools. Practices may spend $8,000–$15,000+ annually on technology, and total costs can reach $200,000–$350,000+ depending on staff size and tech requirements. This often results in a cost-to-collect rate of about 13.7 % of collections.
Pros
- Full control of billing processes and staff workflows.
- Immediate access to the internal team for questions and issue resolution.
- Better integration with clinical staff and practice operations.
Cons
- Significantly higher overhead, like salaries, benefits, and recruitment costs.
- Staff turnover, training, and staying current with coding/ payer rules is expensive and disruptive.
- May lack specialized billing expertise in complex nephrology coding.
Outsourced Nephrology Billing Model
Outsourced medical billing means partnering with a third-party nephrology medical billing company or RCM provider. These teams handle all revenue cycle tasks from coding and submission to denials and follow-up, using advanced tools and expertise.
Price (Typical Costs)
Outsourced billing fees are usually based on a percentage of collections, typically around 4–8 % of monthly net revenue. For example, a practice generating $1 million in annual collections might pay $30,000–$90,000 per year for outsourced billing services. This cost is usually much lower than in-house costs.
Pros
- Lower operational costs with no salaries, benefits, or internal training required.
- Access to certified coders and billing specialists who stay current with CPT/ICD-10 changes.
- Typically results in higher clean claim rates and fewer denials.
Cons
- Less direct control over day-to-day billing operations and immediate decisions.
- Possible communication delays if vendor responsiveness is not strong.
- Vendor quality varies, so choosing a reliable partner is critical.
How to Choose the Right Nephrology Medical Billing Partner?
Choosing the right nephrology billing partner can make a significant difference in your cash flow. The following criteria will help you make an informed decision:
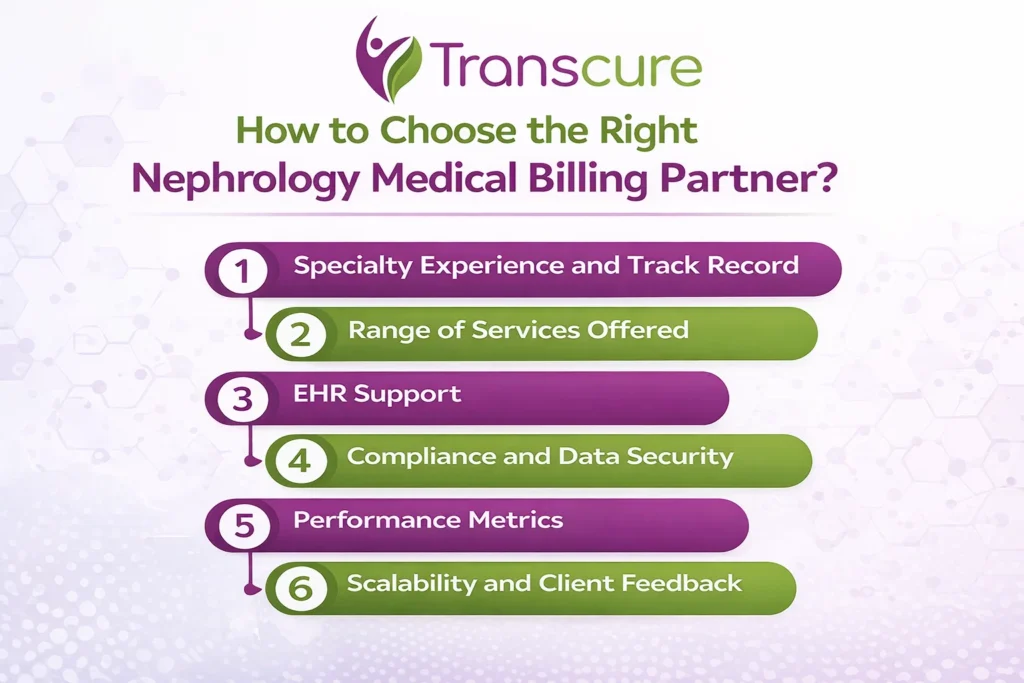
1. Specialty Experience and Track Record
Look for a billing partner with proven experience in nephrology billing and kidney care coding. A partner familiar with CPT and ICD-10 codes specific to chronic kidney disease, ESRD, and dialysis is more likely to reduce denials and improve reimbursements. Ask about their work with practices similar to yours and request client references if possible.
2. Range of Services Offered
A strong nephrology billing partner should provide end-to-end revenue cycle management, not just claims submission. This includes eligibility verification, coding, denial management, payment posting, A/R follow-up, and regular reporting.
3. EHR Support
Ensure the billing company uses modern billing software and can integrate with your practice’s EHR/EMR systems. Confirm which nephrology-specific EHRs they support, such as systems used for dialysis centers, lab reporting, and care coordination.
4. Compliance and Data Security
Handling patient data requires strict HIPAA compliance and robust security protocols. Ask how the partner protects patient information with encryption, secure transfers, and regular audits. A partner who prioritizes data security helps safeguard your practice from legal and financial risks.
5. Performance Metrics
Most importantly, ask the nephrology billing agency regarding its performance metrics, including first-pass clean claim rates and AR days. Moreover, make sure the company provides transparent, regular performance reports and clearly defines accountability for revenue outcomes.
6. Scalability and Client Feedback
Last but not least, a good billing partner should be able to scale services with your practice, whether you add providers, locations, or services. Plus, read verified client reviews, testimonials, and case studies.
Conclusion
In conclusion, these advanced strategies provide a comprehensive guide to elevate your nephrology coding and billing practices. Staying informed about code changes, ensuring compliance, leveraging technology, and considering outsourcing are key components to optimizing revenue and streamlining operations in your nephrology practice.
FAQS
1. Which payers are most common in nephrology billing?
Medicare is the primary payer for most ESRD and dialysis patients, followed by Medicaid and commercial insurance plans. Each payer has distinct coverage, bundling, and documentation requirements that must be followed carefully.
2. Can lab services be billed separately in nephrology?
Some lab services can be billed separately when they are not included in the ESRD PPS bundle. Proper documentation and payer-specific rules must be reviewed to avoid denials or overpayments.
3. What is the difference between ESRD PPS and MCP billing?
ESRD PPS applies to facility-based dialysis services and includes bundled payments for most dialysis-related items. MCP billing covers the physician’s monthly management services for ESRD patients.
4. How many dialysis sessions are typically covered per month?
Medicare typically covers up to thirteen dialysis treatments in a standard 30-day month. Additional sessions require clear medical necessity documentation to receive reimbursement.